Not all full-field digital mammography (FFDM) systems are created equal, according to a new analysis of data from the Digital Mammographic Imaging Screening Trial (DMIST). The new study found that radiologists using certain FFDM devices reported improved lesion visibility, according to results published in the August issue of Radiology.
The DMIST study, sponsored by the American College of Radiology Imaging Network (ACRIN), compared FFDM to film-screen mammography in 50,000 asymptomatic women who presented for screening mammography at 33 sites in the U.S. and Canada. Original results were published in the New England Journal of Medicine in September 2005: Researchers found that FFDM was superior to analog mammography for detecting cancer in younger women, though there was no difference between the two technologies for screening in the general population.
In this latest look at DMIST data, Dr. Etta Pisano and colleagues sought to determine which factors contributed to DMIST's cancer detection results in a study published in Radiology (August 2009, Vol. 252:2, pp. 348-357). Pisano's team used 307 DMIST cancer cases with both digital and film-screen mammograms available for the study. Of these 307 cases, 294 had one cancer and 13 had two, giving a total of 320 cancers to review.
Digital mammography was performed with five systems from four manufacturers: SenoScan (Fischer Imaging, Denver; no longer commercially available); FCRm (Fujifilm Medical Systems USA, Stamford, CT); Senographe 2000D (GE Healthcare, Chalfont St. Giles, U.K.); Selenia (Hologic, Bedford, MA); and the Lorad/Trex Digital Mammography System, subsequently replaced by Selenia.
Seven radiologist readers participated in the study -- all had experience using GE's system, and all but one had experience with more than one digital mammography system. The readers knew that all cases had known malignancies, and they rated the relative visibility of these cancers on the film-screen mammograms versus the digital ones, grading visibility on a five-point scale.
The radiologist readers' opinions of the relative visibility of the cancers and the reasons for the differences in visibility between film-screen and digital mammography varied widely, Pisano and colleagues wrote. For cancers in dense and fatty breasts, the most frequent reason cited for variability in lesion visibility between the two modalities was contrast differences. The better visibility of all cancers in the digital mammography images was attributed to image contrast in 161 out of 221 opinions (72.8%); in film-screen images, 133 of 232 opinions (57.3%).
Radiologist reasons for better cancer visibility with one modality rather than the other, for all reviewed cancers
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Note -- Data are numbers of cases of the given reason that cancer lesion visibility was better with one modality rather than
the other, as cited for all analyzed cancers according to case review visibility results. Numbers in parentheses are percentages. * When the reason "other lesion characteristics were more evident" was cited, the reader was asked to provide details. Table and images courtesy of the Radiological Society of North America. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||
The contrast differences were tied to particular devices, the researchers found. For example, the radiologists using the GE system were more likely to rate lesions as more visible on digital images versus analog, compared to those radiologists using the Fuji or Fischer systems, regardless of patient age and breast density. Film-screen mammography was more likely to be rated as better, as opposed to the two being judged equally, when radiologists were viewing Fischer images.
"The decrement in lesion visibility in the fatty breasts with digital mammography that was attributed to image contrast was most marked for those cases acquired using the Fischer system," Pisano and colleagues wrote.
The authors suggested that newer image processing algorithms available with the GE unit at the time of the DMIST study might explain the difference in opinion among readers. In addition, the Fischer system used 12-bit digitization compared to 14 bits used on the other models, and the unit also lacked automatic exposure control, requiring technologists to guess the breast density to set exposure levels. With respect to the Hologic units, the researchers said that their analysis included few cancers detected with those systems, which reduced the power of the study for them.
 |
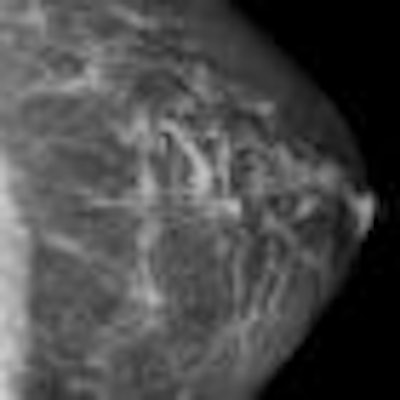
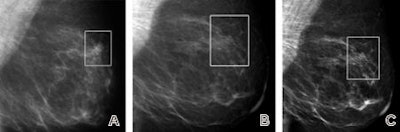
| Craniocaudal mammographic views of dense left breast in 52-year-old-woman. Full digital mammogram obtained by using Senographe system (above, left) and close-up view (below, left) of area outlined (in rectangle), as compared with full film-screen mammogram of same breast (above, right) and close-up view (below, right) of area outlined (in rectangle), reveal how improved contrast in dense part of the breast depicted on the digital mammogram enables visualization of the cancer, an invasive ductal carcinoma, on the digital image but not on the film-screen image. The lesion was not visible on either the mediolateral oblique film-screen or digital mammograms. |
 |
But how can digital mammography yield contrast superior to film-screen in women with dense breasts, while showing inferior contrast in women with fatty breasts? Pisano's team attributed this to factors such as the choice of the x-ray spectrum, the efficiency of the x-ray scatter rejection, and display image processing -- elements that varied by machine type.
"The nature and quality of the image data processing varied considerably," the authors wrote. "The visibility of lesion features is influenced substantially by the image processing algorithm and whether the lesion lies within a dense or fatty background. We believe that this is the most likely explanation for the conflicting results for dense and fatty breasts."
 |
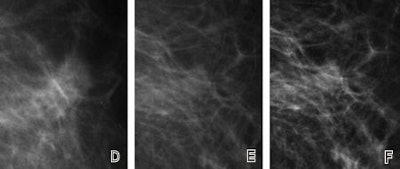 |
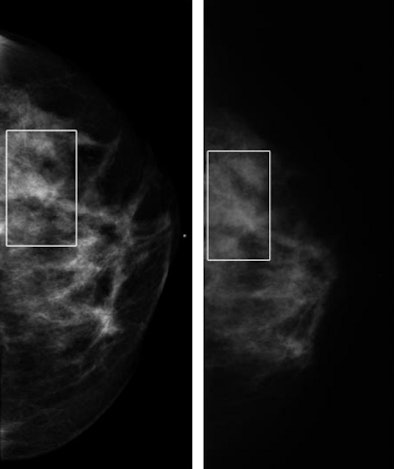
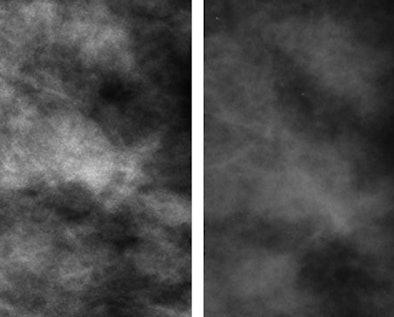
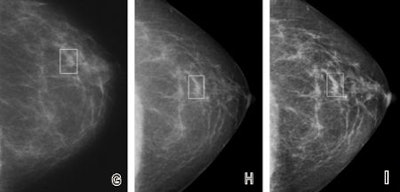
| Fatty breast depicted on (A, D, G) film-screen and (B, C, E, F, H, I) digital left mammograms obtained in 53-year-old woman. Cancerous areas are outlined in rectangles. (A-F) Mediolateral oblique and (G-I) craniocaudal views are shown. The cancer, a mass that proved to be an invasive ductal carcinoma, is much more apparent on the film-screen images than on the digital images, with visibility being greatest on the film-screen mediolateral oblique views. The difference in lesion visibility between the film-screen and digital mammograms is accentuated when the film-screen overview image (A) is compared with the digital overview image obtained by using the default image processing algorithm (B). Close-up views of cancerous areas outlined in A (D) and B (E) are shown. There is a slight improvement in the visibility of the lesion depicted at digital mammography performed by using the Premium View image processing software, as seen on digital mediolateral oblique overview (C), film-screen mediolateral oblique close-up view (D), and digital craniocaudal (I) images. |
 |
The team's hypothesis was that digital mammography manufacturers concentrated on designing image processing algorithms to improve grayscale in dense breasts, while de-emphasizing optimal image processing in fatty breasts: justified, perhaps, since film-screen misses more cancers in dense breasts.
"Our study demonstrates that the results obtained in DMIST were not due primarily to accidents in positioning or interpretation," Pisano and colleagues wrote. "That is, digital mammography performed significantly better in particular subsets of women because of the better conspicuity of lesions in those subgroups. Screen-film mammography tended nonsignificantly to perform better in the subset of women aged 65 years or older with fatty breasts.... This suggests that digital system manufacturers should improve the quality of their image processing algorithms, especially for fatty breasts."
By Kate Madden Yee
AuntMinnie.com staff writer
July 27, 2009
Related Reading
FFDM equals analog mammography in hard-copy reading, May 7, 2009
CAD boosts FFDM performance, March 4, 2009
FFDM performs well versus analog for screening, studies show, January 6, 2009
Digital mammograms take longer to read, study suggests, January 6, 2009
DMIST: Women under 50 with dense breasts benefit from FFDM, January 29, 2008
Copyright © 2009 AuntMinnie.com