With the clinical success of intensity-modulated radiotherapy (IMRT), research is now focused on optimizing and evolving IMRT techniques. Three distinguished medical physicists recently examined the current state of the art and future directions in advanced IMRT planning, quality assurance (QA), and image guidance.
Thomas Bortfeld, PhD, director of the physics division of Massachusetts General Hospital's department of radiation oncology, discussed the ongoing evolution of IMRT at the American Association of Physicists in Medicine (AAPM) and Canadian Organization of Medical Physicists (COMP) joint meeting held earlier this month in Vancouver, British Columbia. The symposium was dedicated to the memory of radiation oncology pioneer Dr. Steven Leibel.
Bortfeld explained that in the 1990s, IMRT was delivered by either conebeam or fanbeam techniques, noting that "conebeam delivery using a multileaf collimator proved to be the winner." Today, however, the landscape is far more complex. Developments in conebeam IMRT have led to techniques such as volumetric-modulated arc therapy (VMAT) and RapidArc (Varian Medical Systems), while advances in fanbeam IMRT enabled the evolution of helical tomotherapy.
"I was skeptical at the start of the development of VMAT, but I'm now convinced by the results that have come out recently," said Bortfeld. "The key advantage is greater efficiency."
He cited several papers showing the benefits of VMAT/RapidArc, including a study in which VMAT was able to provide a 40% reduction in treatment time while maintaining comparable plan quality to that of helical tomotherapy. Bortfeld pointed out, however, that tomotherapy is still the better option for highly complex cases.
"So tomotherapy planning is the gold standard, but VMAT is usually the most time-efficient method," Bortfeld explained. "The question is, can we get the best of both worlds?"
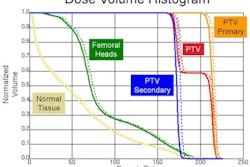
The answer is yes, and the solution lies in the use of multicriteria optimization (MCO), an approach that's currently being investigated at Massachusetts General Hospital. Multicriteria optimization-based treatment planning works by generating a set of Pareto plans, which then can be used to determine the best compromise between specified clinical and planning criteria.
Multicriteria optimization can reduce IMRT planning time by an order of magnitude versus standard techniques. But, according to Bortfeld, it's VMAT planning, which is more challenging than fixed-field IMRT, where multicriteria optimization could really make an impact.
"I hypothesize that advanced planning techniques like MCO will be able to make improvements for VMAT by substantially reducing the treatment planning time, and also helping us understand more about the trade-offs between quality and efficiency," he said.
Bortfeld pointed out that multicriteria optimization offers plan quality that's practically indistinguishable from the gold standard of tomotherapy. "Developments in VMAT planning are needed for greater efficiency of planning, to guarantee uncompromised dosimetric quality and high delivery efficiency," he concluded. "In my opinion, MCO promises to accomplish all that."
QA quandary
The topic of quality assurance issues surrounding advanced IMRT was discussed by Thomas LoSasso, PhD, a medical physicist at Memorial Sloan-Kettering Cancer Center. "Since the early years of IMRT, it has been my position that dose measurements should not be a requirement for patient-specific IMRT QA," he stated. Instead, it's preferable to be more confident in the treatment system's performance in the first place.
IMRT errors can be divided into two types, LoSasso said. Physical errors, such as incorrect calibration, result in deviations of typically less than 10%. Catastrophic errors such as delivery to the wrong field, on the other hand, can lead to errors of two to four times the expected dose. LoSasso's proposition is that if the treatment planning system can accurately simulate beam delivery, and targeted machine QA is performed, then patient-specific QA is only needed to detect infrequent catastrophic errors -- and these don't require dose measurements to be detected.
Characteristics of the beam delivery system, such as leaf offset, multileaf collimator leakage, multicomponent source, and tongue-and-groove effects, are all major contributors to uncertainties in measurement-based IMRT quality assurance. "These need to be accurately modeled in the treatment planning system, or you will end up with errors," he said. But with an accurately commissioned planning and delivery system, this approach can reduce time and effort requirements when dealing with large numbers of IMRT patients.
LoSasso concluded with some suggestions for the future. He recommended that vendors of treatment planning systems should accurately model IMRT-sensitive multileaf collimator parameters and provide default values for these parameters. Linear accelerator vendors, meanwhile, should provide software tools to manage performance verification. He also proposed that AAPM Task Group recommendations for patient-specific quality assurance should acknowledge alternative QA methods.
Future focus
C. Clifton Ling, PhD, laboratory head of molecular pharmacology and chemistry at Memorial Sloan-Kettering Cancer Center and director of advanced clinical research for oncology systems at Varian Medical Systems, discussed future directions in IMRT with a focus on image-guided radiotherapy (IGRT). He explained that 20 years ago radiotherapy was controlled from a simple console. Now, with the plethora of available image-guidance techniques, control setups are highly complex with far too many consoles per treatment system.
Integration of image-guidance devices into the treatment planning process can increase efficiency, streamline workflow, and enable automatic QA, said Ling, citing Varian's TrueBeam system that has one control system for everything.
He also pointed out that with so many image-guidance options available, one major challenge today is how to select the most suitable equipment and integrate it into the workflow. As it's not possible to perform clinical trials for every new image-guidance device, this choice must be based on surrogates, such as setup error reduction and organ motion compensation, rather than clinical outcome data.
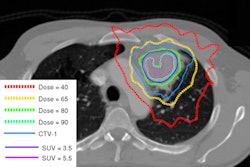
Looking to the future, Ling surmised what may come next. "IGRT, more IGRT," he said, noting that one possibility could be the development of biological image-guided adaptive radiotherapy, or BIGART. He emphasized that while biological images provide a wealth of information, it's vital to understand exactly what all the images mean. "We need to quantify the impact of biological features and better understand the characteristics of normal tissue," he pointed out.
So are we going to see biological-based guidance modalities such as BIGART entering clinical practice? "I think so," Ling concluded, "but the time frame is really hard to predict; maybe five to 10 years, maybe 10 to 15."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community Web site covering fundamental research and emerging technologies in medical imaging and radiation therapy.