A diffusion-weighted MRI (DWI-MRI) brain sequence can confirm the presence of acute stroke within a few days after low-risk stroke patients present with seemingly minor symptoms, according to an international six-year study published September 23 in JAMA Neurology.
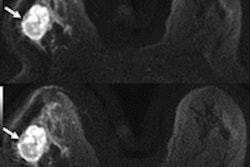
Researchers used axial DWI-MRI to accurately diagnose acute stroke within eight days in individuals who were suspected of having a low-risk transient ischemic attack (TIA) because of minor symptoms, but who didn't have the motor and speech problems typical of an actual stroke. DWI-MRI showed that 13% of these patients actually had experienced strokes -- and were six times more likely to have a recurrent stroke in the subsequent year, a number that surprised the researchers.
"The implication of this finding is that if the diagnosis of TIA or minor stroke is considered, even with low-risk features, early MRI must be completed within one week to make a definitive diagnosis of ischemic stroke," wrote the authors, led by principal investigator Dr. Shelagh Coutts, a neurologist with the University of Calgary Cumming School of Medicine. "A simple short-sequence brain MRI (e.g., axial DWI, fluid-attenuated inversion recovery, or gradient recalled echo) is typically adequate."
Of the 500,000 or so North Americans who experience a TIA or minor stroke annually, about 50% have symptoms that mimic a stroke but generally have a more benign prognosis. On the other hand, it is estimated that 10% to 17% of these individuals will experience a recurrent stroke within 90 days. The key is finding out which ones.
Hence, clinicians have turned to DWI-MRI to visualize ischemia, arterial blockage, or stenosis, and single out the patients with the greatest risk of an early recurrent stroke.
In this study, the researchers prospectively collected data from 1,028 patients (mean age, 63.0 ± 11.6 years) who presented with low-risk symptoms, such as numbness, dizziness, very short episodes of weakness, or speech difficulties, at a total of nine facilities in Canada, Australia, and the Czech Republic. Subjects were enrolled no later than eight days after the onset of symptoms (median time, 102 hours; range, 53-144 hours) and before their 1.5- or 3-tesla DWI-MRI scans to ensure image acquisition of all small diffusion lesions.
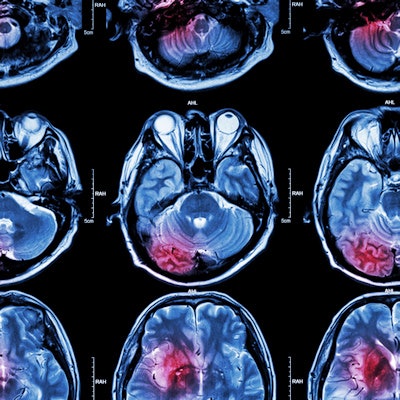
The scans revealed acute infarcts in the form of DWI-positive lesions in 139 participants (13.5%). Among them, 92 participants (8.9%) had a single lesion and 47 (4.6%) had multiple lesions. DWI-MRI also revised stroke diagnoses in 308 patients (30%).
At one-year follow-up, seven patients had recurrent strokes (0.7%), with DWI-positive lesions associated with an increased risk of the event (relative risk, 6.4). Conversely, patients with no DWI-positive lesions achieved a negative predictive value of 99.8% and had no recurrent stroke.
"The failure to make a correct diagnosis of stroke results in a missed opportunity for stroke prevention and the incorrect diagnosis of stroke results in use of therapy that has the capacity to harm," Coutts and colleagues added. "Long-term antiplatelet therapy with aspirin in the healthy elderly is harmful. Clinical judgment will continue to be required to decide which patients with DWI-negative MRI findings require preventive treatment."