Preoperative needle biopsies in patients who undergo surgery for lung cancer are associated with an increased risk of cancer recurrence, according to a study published October 14 in Radiology.
The finding is from an analysis of outcomes among 783 patients who underwent CT-guided percutaneous transthoracic needle biopsy prior to sublobar resection and 1,243 patients who did not and confirms concerns about “tumor cell spillage” during the procedure, noted lead author Yura Ahn, MD, of Asan Medical Center in Seoul, South Korea.
“With the increasing adoption of sublobar resection as a standard approach for early-stage lung cancer, tumor cell spillage is becoming a potential concern,” the group wrote.
Percutaneous transthoracic needle biopsy (PTNB) is a widely used diagnostic method for characterizing pulmonary lesions to help plan surgeries, with high accuracy and safety, the authors explained. However, PTNB may increase the risk of tumor cell dissemination along the biopsy tract, they wrote.
While rare, this so-called track seeding has been consistently reported following percutaneous biopsy in hepatocellular carcinoma, renal cell carcinoma, and breast cancer, but to date the link has not been evaluated in patients undergoing sublobar resection, the group noted.
The researchers retrospectively analyzed outcome data for 2,026 patients with stage I non–small cell lung cancer (tumor size ≤ 3 cm) who underwent sublobar resection between January 2010 and December 2021. PTNB was performed in 783 patients (38.6%), while the remaining 1,243 patients (61.4%) underwent surgery without PTNB.
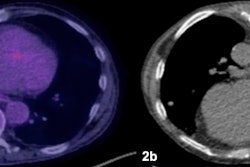
 Remnant lung recurrence after percutaneous transthoracic needle biopsy (PTNB) following wedge resection. (A) Preoperative contrast-enhanced axial CT scan in a 76-year-old male patient shows a 1.8-cm solid nodule in the left upper lobe (arrow). (B) The patient underwent PTNB for nodule diagnosis. A nonenhanced axial CT scan showed that the introducer needle (arrowheads) was inserted into the inner portion of the nodule (arrow), traversing the lung parenchyma. The diagnosis on the basis of results from the PTNB was adenocarcinoma, and the patient subsequently underwent left upper lobe wedge resection 7 days after PTNB was performed. The final diagnosis was adenocarcinoma of the solid-predominant type, pT1bN0. (C) At postoperative follow-up, a nodular opacity emerged adjacent to the surgical site (arrowheads) and increased in size at subsequent imaging. This soft-tissue lesion was confirmed at PTNB as metastatic adenocarcinoma, and the patient underwent salvage radiation to treat the remnant lung recurrence.RSNA
Remnant lung recurrence after percutaneous transthoracic needle biopsy (PTNB) following wedge resection. (A) Preoperative contrast-enhanced axial CT scan in a 76-year-old male patient shows a 1.8-cm solid nodule in the left upper lobe (arrow). (B) The patient underwent PTNB for nodule diagnosis. A nonenhanced axial CT scan showed that the introducer needle (arrowheads) was inserted into the inner portion of the nodule (arrow), traversing the lung parenchyma. The diagnosis on the basis of results from the PTNB was adenocarcinoma, and the patient subsequently underwent left upper lobe wedge resection 7 days after PTNB was performed. The final diagnosis was adenocarcinoma of the solid-predominant type, pT1bN0. (C) At postoperative follow-up, a nodular opacity emerged adjacent to the surgical site (arrowheads) and increased in size at subsequent imaging. This soft-tissue lesion was confirmed at PTNB as metastatic adenocarcinoma, and the patient underwent salvage radiation to treat the remnant lung recurrence.RSNA
The median follow-up duration for recurrence was 46.5 months, with a median of 44.4 months in the non-PTNB group and 51.6 months in the PTNB group. The outcomes evaluated were freedom from overall recurrence, specific recurrence patterns (local-regional, distant, remnant lung, and ipsilateral pleural recurrence), and overall survival.
In the group that underwent PTNB, the procedure was associated with a greater risk of overall recurrence (hazard ratio [HR], 1.49; p = 0.03) and local-regional recurrence (HR, 2.32; p = 0.008), without evidence for distant recurrence (p = 0.29), the researchers reported.
Among local-regional recurrences, PTNB was linked to an increased risk of remnant lung recurrence (HR, 2.07; p = 0.03) but not to ipsilateral pleural recurrence (HR, 1.13; p = 0.79), they noted. Lastly, there was no evidence of an association between PTNB and overall survival, according to the results.
“Percutaneous transthoracic needle biopsy was associated with local-regional recurrence, particularly in the remnant lung, in patients with stage I non–small cell lung cancer who underwent sublobar resection,” the group wrote.
The authors noted that further prospective investigations are necessary to validate the findings and clarify their clinical implications.
In an accompanying editorial, Jae Ho Sohn, MD, and E. Han Dao, MD, of the University of California, San Francisco, wrote that the results confirm the biologic plausibility that biopsy may displace malignant cells into the nearby lung parenchyma, where they persist after limited resection. Yet the results do not warrant abandoning biopsy altogether, and PTNB remains important in several contexts, they noted.
“PTNB is important when there is diagnostic uncertainty at imaging, as biopsy can prevent unnecessary surgery in patients with benign nodules,” Sohn and Dao wrote.
In addition, PTNB can be used to help manage patients who are not candidates for surgery, as biopsy can establish diagnosis to help with clinical decision making for systemic or radiation therapy, they added.
“Nonetheless, acknowledging this potential association during pre-biopsy discussions may help align patient expectations and support shared decision-making,” the two concluded.
The full study is available here.