Stent placement does not appear to reduce the risk of recurrent strokes compared with medical therapy in patients with narrowing of arteries in the brain, according to a study published July 1 in Radiology.
The finding is from a prospective trial in China in patients with intracranial atherosclerotic stenosis (ICAS) and supports similar findings from earlier trials, noted lead author Bonaventure Ip, MD, of The Prince of Wales Hospital in Hong Kong, and colleagues.
“The results of our study support the current recommendations of medical therapy over stenting for secondary stroke prevention in patients with symptomatic ICAS,” the group wrote.
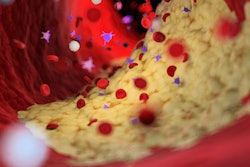
ICAS is caused by the build-up of plaque in the arteries due to atherosclerosis and is a major cause of ischemic stroke with a risk of recurrence. Endovascular revascularization therapy (stenting) has been hypothesized as a treatment, yet previous trials have shown little benefit of the procedure over medical therapy, the authors noted.
However, previous trials included patients with concurrent branch atheromatous disease adjacent to the stent target, with these patients being at higher risk of complications during the procedure, they added. In this study, to further evaluate the use of stenting in ICAS, the researchers first excluded patients with branch atheromatous disease using three-dimensional rotational angiography.
The study included 150 participants (mean age, 61 years old, 45 women) with transient ischemic attack or ischemic stroke attributed to severe ICAS who were randomized into stenting (n = 74) and medical therapy (n = 76) groups. The primary end point was a composite of transient ischemic stroke, ischemic stroke, intracranial hemorrhage, and death within 30 days or any ischemic stroke from 30 days to one year.
According to the results, stenting did not result in a reduction in ischemic stroke cumulative incidence compared with medical therapy with antiplatelet drugs at one year (stenting versus medical therapy: 12 of 74 [16%] vs. 18 of 76 [24%], p = 0.26). Stenting also did not reduce the cumulative incidence of ischemic stroke compared with medical therapy over a 10-year follow-up period, the researchers reported.
“Intracranial stenting did not result in a reduction in the cumulative incidence of stroke or death at 30 days or stroke from 30 days to one year,” the group wrote.
To date, despite considerable efforts to introduce endovascular revascularization therapy for severe ICAS, no randomized control trial has shown its benefits over intensive medical therapy, the authors noted. Ultimately, further studies with larger sample sizes are needed to substantiate the findings, the researchers concluded.
In an accompanying editorial, Joan Wojak, MD, of Louisiana State University School of Medicine in New Orleans, noted that primary stent placement has become a focus due to its historical success compared with angioplasty alone in patients with coronary artery disease. The long struggle to develop effective endovascular therapy (thrombectomy, for instance) in patients with coronary artery disease ultimately resulted in disruptive evolution and the widespread acceptance of the therapy, she wrote.
“Establishing a role for endovascular therapy in the treatment of symptomatic intracranial atherosclerotic stenosis has proved to be even more elusive,” Wojak concluded.
The full study can be found here.