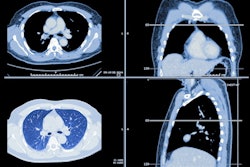
A follow up analysis of the ELCAP-coronary artery calcium (CAC) scoring system (ELCAP-CAC) used with low-dose CT (LDCT) imaging has shown that the framework is effective for predicting death from cardiovascular disease (CVD).
The findings show that "a single ELCAP-CAC score at LDCT is a powerful long-term predictor of CVD death," according to a team led by Joseph Shemesh, MD, of Sheba Medical Center in Ramat Gan, Israel, and "brings to light the potential for combining early detection of CVD and lung cancer, which are the top causes of death in the United States."
Shemesh and colleagues noted that, in 2006, researchers introduced a 12-point visual ordinal ELCAP-CAC score for nongated LDCT. This scoring system has been shown to be a strong predictor of cardiovascular disease (CVD) death. In this analysis, the authors assessed whether the framework is still a strong predictor of CVD and all-cause mortality after a longer follow-up (through December 2024).
The research included 8,782 individuals who underwent LDCT screening between 2000 and 2004 (of these, 2,506 participants were from Weill Cornell Medicine in New York and 6,276 participants were from the New York Early Lung Cancer Action Program, or NY-ELCAP). All those who participated in the study were current or former smokers between the ages of 40 to 85 years.
Radiologists at each institution categorized the LDCT exam results using ELCAP-CAC scoring (0, 1 to 3, and 4 to 12, corresponding to low, intermediate, and high risk, respectively). Four chest radiologists with experience ranging from seven to 28 years reviewed these scores. The researchers tracked study participant outcomes via the National Death Index and cause of death was coded as either CVD or non-CVD, and calculated follow-up time from baseline LDCT to time of death or December 2024, tracking patterns of mortality risk with Cochran-Armitage trend tests. They also estimated incidence of CVD and all-cause mortality using the Kaplan-Meier method, and adjusted these models for sex, age, pack-years of smoking, and diabetes.
During a median follow-up of 23 years, 3,705 participants (42.2%) died. Of these deaths, 1,146 (30.9%) were caused by CVD. Cumulative incidence of CVD deaths increased by CAC categories of 0 (9.4%), 1 to 3 (16.5%), and 4 to 12 (30.5%) and was statistically significant (p< 0.0001); this trend was also seen for all-cause mortality.
The investigators also noted the following:
- CVD deaths were higher for ELCAP-CAC 4 to 12 compared with ELCAP-CAC 0 (hazard ratio, or HR, of 3.68, with one as reference; p< 0.0001). This trend was also found for all-cause mortality (HR, 2.85, p<0.0001).
- The risk of CVD death increased with higher CAC categories for all age groups (<60 years, 60 to 69 years, and ≥70 years).
The study results confirm the efficacy of the ELCAP-CAC scoring system, according to the investigators, who wrote that the framework "enhances the benefit of chest CT screening as it provides clinicians, including cardiologists or general practitioners, with an additive powerful predictor of CVD death that improves on traditional laboratory-based methods of CVD risk assessment."
"As the longest prospective study of CVD risk in lung cancer screening participants, our study demonstrates that a baseline ELCAP-CAC score is strongly predictive of CVD and all-cause mortality up to 25 years," they concluded. "In the era of artificial intelligence–enabled opportunistic screening, combined early detection of CVD and lung cancer using LDCT presents a major opportunity to advance public health and preventive medicine."
The complete report can be found here.