SAN DIEGO - Brain tumors are among the fastest growing cancers, with some of the highest mortality rates. These traits make imaging vital for the prompt assessment of tumor recurrence and radiation necrosis in staging and patient management. And because the major dose-limiting complication of radiotherapy to the brain is radiation injury, accurately determining necrosis is critical for patient survival.
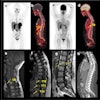
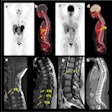
At the 2002 Academy of Molecular Imaging conference last week, Dr. Miguel Pozo of the Centro PET Complutense in Madrid offered compelling evidence of the accuracy of FDG-PET imaging with MRI co-registration versus MRI alone in resolving diagnostic doubt between brain tumor recurrence and post-treatment radionecrosis.
Pozo led a team of researchers that evaluated 94 patients with central nervous system tumors. The patients presented with 31 low-grade and 39 high-grade astrocytomas, 3 oligondendrogliomas, 13 metastatic tumors, and 8 tumors of other types. All the patients had undergone radiotherapy as well as other treatments such as radiosurgery, chemotherapy, or other types of surgery.
The group then set out to evaluate the accuracy of MRI and FDG-PET with MRI co-registration. The images were taken with separate scanners and co-registered with MRI via software.
In the FDG-PET studies, the team performed both visual and semi-quantitative analysis based on the standardized uptake value of FDG in the tumors. Visual differentiation in the PET studies was determined by a recurrent tumor exhibiting hypermetabolism of glucose, a non-necrotic irradiated brain showing hypometabolism, and a necrotic brain showing no detectable metabolic activity.
The findings, 43 instances of recurrent tumors and 51 instances of radionecrosis, were confirmed either clinically (80%) or histologically (20%) in all the cases.
In the evaluation of FDG-PET and MRI co-registration and solitary MRI for necrosis, MR images were labeled as necrotic in 5 instances, as recurrent tumor in 6 instances, and as inconclusive or doubtful in 40 instances. The results of FDG-PET and MRI co-registration were deemed necrosis in 50 instances, and as recurrent tumor in one, with no inconclusive findings.
In the 43 instances of recurrent tumors, MR imaging resulted in a diagnosis of necrosis in 4 instances, as recurrent tumor in 4, and as inconclusive or doubtful in 35 studies. The FDG-PET and MRI correlation resulted in one case being called necrosis, and 42 studies classified as recurrent tumor, with no inconclusive findings.
Because the MRI findings resulted in 75 out of 94 instances of doubtful or inconclusive findings while the co-registration of MRI with FDG-PET provided a correct diagnosis in 92 patients (81 true positive, 11 true negative, 1 false positive, and 1 false negative), Pozo believes that the modalities should be combined whenever a clinician is differentiating brain tumor recurrence from radionecrosis.
"We found that MRI and FDG-PET alone are unable to obtain a correct diagnosis in this common clinical situation, but the combination of the two provided superior accuracy," Pozo said.
According to Pozo, the use of FDG-PET and MRI together provided a sensitivity of 97.6% and a specificity of 98%. The positive predictive value was 97.6%, negative predictive value was 98%, and a total accuracy of the combined approach was 97.8% in this study. The researchers plan to conduct further studies to evaluate the accuracy of the standardized uptake value as a prognostic factor for survival in patients with brain tumors.
"We found that the metabolic images obtained with FDG-PET are superior to anatomo-structural imaging techniques in providing a differential diagnosis to distinguish between tumoral recurrence and radionecrosis in central nervous system tumors that have undergone therapy," Pozo stated.
By Jonathan S. BatchelorAuntMinnie.com staff writer
October 29, 2002
Related Reading
Gliomas well-defined with proton MR spectroscopy, April 16, 2002
MRI and SPECT garner high marks for glioma grading, March 5, 2001
MR perfusion helps diagnose brain lesions, February 16, 2001
Copyright © 2002 AuntMinnie.com