For many nuclear cardiologists, SPECT imaging is the workhorse technology for assessing myocardial viability. But PET and MRI are also making headway in the offices of cardiac imaging specialists. These experts gathered to discuss the strengths and weaknesses of each modality during a session at the 2002 American Society of Nuclear Cardiology meeting in Baltimore.
Though the session was framed as a debate, the speakers spent little time attacking other technologies, agreeing that the expertise of a specific center -- be it in nuclear medicine or non-nuclear techniques -- should guide patient care, more than dedication to a specific technology.
SPECT and MRI
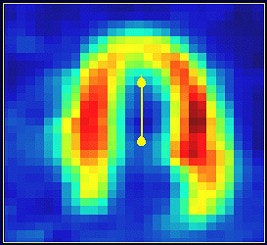
Dr. Dudley Pennell, a cardiologist and MR expert at the Royal Bromptom Hospital in London, stumped for MRI. Its advantages include speed, lack of radiation, and high-resolution images, he said.
"Magnetic resonance has advantages of comprehensiveness. This will be used increasingly for the assessment of viability," he said.
Recent reports would seem to bear out Pennell’s assessment. Researchers from Wake Forest University School of Medicine in Winston-Salem, NC, found that in patients with poor echocardiogram results, MRI, combined with dobutamine/atropine cardiac stress testing, could pinpoint inducible ischemia, generally associated with a higher risk of myocardial infarct or cardiac death (Circulation: Journal of the American Heart Association online, October 14, 2002).
And at the 2002 Society of Nuclear Medicine conference in Los Angeles, German investigators reported that late-enhancement MRI offers a reasonable alternative to FDG-PET for assessing myocardial viability. The modality seems particularly adept at detecting tissue that has irreversible damage, the group said.
But the major factor that could limit the use of MR for cardiac assessment is the lack of experts available to perform and interpret the scans, according to Pennell. "The scanners are available. The expertise is not," he said. "Like lots of techniques, there are grades of difficulty."
In comparison, "SPECT is a mature technology that people use for different reasons every day. There’s SPECT equipment in (cardiologist’s) offices. SPECT and dobutamine echo -- they work, and people have (the equipment)," commented session moderator Dr. James Udelson, the director of nuclear cardiology at the Tufts-New England Medical Center in Boston.
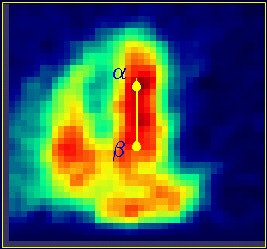
SPECT and FDG-PET
The same lack of expertise limiting MRI's scope is likely to arise with PET scans to assess viability, Udelson said.
Dr. Paolo Camici, professor of cardiovascular pathophysiology at Imperial College of Science, Technology and Medicine in London, spoke on behalf of PET scanning in heart-disease patients. He noted that FDG-PET allows for the assessment of blood flow and glucose metabolism, especially in patients with the most severe heart failure, and praised FDG-PET’s ability to stratify patients on the basis of risk.
  |
"Above all," he said, "it allows you to achieve qualitative measurements."
FDG-PET's advantages over SPECT include higher sensitivity, higher specificity, and the ability to measure myocardial blood flow, as well as myocardial metabolism. The latter is important for understanding the pathophysiology of ischemic cardiomyopathy (Nuclear Medicine Communications, April 2002, Vol. 23:4, pp.323-330).
A group from the Peking Union Medical College in Beijing assessed 123 consecutive patients with previous myocardial infarction (MI) and left ventricular (LV) dysfunction, using FDG-PET and 99mTc-MIBI SPECT. They found both methods to be equally efficient for predicting clinical outcome and determining treatment strategy. Patients with more than 2 viable myocardial segments on imaging were more likely to benefit from revascularization, they reported (Journal of Nuclear Medicine, August 2001, Vol. 42:8, pp.1166-1173).
But the growing use of PET is unlikely to drive doctors away from the familiar terrain of SPECT technology, Udelson said. Cardiac FDG-PET proponents themselves have advocated the standardization of FDG-PET imaging techniques for evaluating myocardial viability.
For instance, researchers at the Turku University Central Hospital in Finland pointed out that "investigations using FDG imaging to predict improvement in left ventricular (LV) function after revascularization have reported wide ranges for sensitivity (71%-100%) and, in particular, for specificity (33%-91%)."
They suggested that multicenter trials are necessary to standardize FDG-PET cardiac protocols and determine whether the modality has value for predicting long-term function, survival, and quality of life (European Journal of Nuclear Medicine and Molecular Imaging, September 2002, Vol. 29:9 pp. 1257-1266).
And some investigators are working toward updating SPECT imaging: Japanese researchers from Hokkaido University Graduate School of Medicine in Sapporo used FDG with SPECT, rather than PET, in patients with ischemic heart disease. This study used FDG-SPECT paired with ultra-high-energy collimators. They found that the agreement between the defect scores based on FDG-SPECT images and FDG-PET images was 70%. The uptake based on FDG-SPECT images significantly correlated with that based on FDG-PET images, they wrote in Nuclear Medicine Communications (September 2002, Vol. 23:9, pp. 879-885).
Outcomes
Whichever modality prevails, nuclear cardiologists are in agreement that proper assessment of myocardial viability is one of the keys to successful treatment. Patients with damaged, but viable, myocardial tissue tend to benefit most from revascularization, while patients with little viable tissue are unlikely to improve -- and may be harmed -- by aggressive intervention.
When it comes to viability studies, "outcomes are the real driver. If you take a patient with poor viability into surgery, they don’t do very well," concluded Dr. Robert Hendel, director of nuclear cardiology at Rush-Presbyterian-St. Luke’s Medical Center in Chicago.
"Do whatever is best in your institution," added Camici. "The important thing is that we do things properly (and) early."
By Brian ReidAuntMinnie.com contributing writer
October 21, 2002
Copyright © 2002 AuntMinnie.com




















