Surgeons should consider breast PET studies to determine if they can skip biopsy and proceed straight to axillary lymph node dissection (AND), according to a study in the Archives of Surgery. But the study authors cautioned that the PET exam must predict positive nodes with 100% specificity.
"The purpose of this article is not to advocate using PET to identify axillary metastasis but to educate physicians that if PET is performed before surgery for systematic staging, a (standard uptake value) should be calculated for axillary activity," wrote Dr. Alice Chung and colleagues from the Saul and Joyce Brandman Breast Center at Cedars-Sinai Medical Center in Los Angeles. Dr. Alan Waxman, chief of nuclear medicine, is a co-author.
"We investigated the use of FDG-PET as part of a strategy for evaluating the axilla in patients with breast cancers of variable sizes and variable characteristics before SNB (sentinel node biopsy) or AND," they explained (Archives of Surgery, August 2006, Vol. 16:8, pp. 783-789).
This retrospective review was based on 462 women with invasive breast cancer who underwent FDG-PET for staging. Of these, 51 had PET scans before axillary surgery or chemotherapy.
PET imaging (Allegro or Gemini, Philips Medical Systems, Andover, MA) was started a little less than two hours after the patient was given 13 mCi of FDG contralateral to the primary tumor. Eight-two percent of the women were imaged in prone and supine positions. SNB was most commonly done with isosulfan blue dye and Tc-99mm-labeled sulfur colloid.
A receiver operating characteristic (ROC) analysis was performed on standard uptake value (SUV) thresholds from 0.5 to 4.0 in 0.2 to 0.3 increments. Positive or negative PET results were based on SUV thresholds and compared with pathologic findings.
Some of the major tumor characteristics based on the results were as follows: 85% of the tumors were invasive ductal carcinoma, 24 were T2 tumors, 74% were estrogen-receptor positive, and the mean tumor size was 3.0 cm.
There were 60 "hot" axillary sites with SUVs ranging from 0.7 to 11. No axillary activity was detected in 41% of the patients. Eleven percent had positive SNB results and went on to AND. Fifty-four percent of the patients underwent AND without SNB.
"When the SUV threshold was 2.3, specificity and PPV (positive predictive value) were 100% and sensitivity and NPV (negative predictive value) were 60% and 53%, respectively," the group wrote.
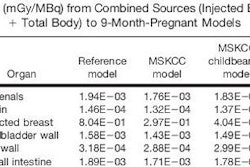
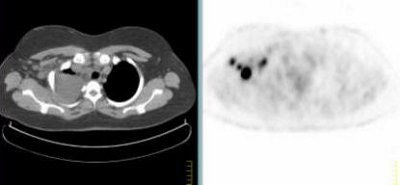 |
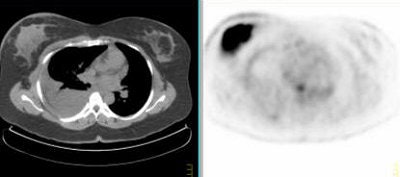
Above, multiple axillary nodal metastases, SUV all > 2.3. Below, primary breast tumor with SUV 7.4. Images courtesy Dr. Alan Waxman.
 |
PET found 60 axillary sites of which 42% were true-positive and 30% were true-negative at the 2.3 SUV threshold. There were no false positives and 28% of the results were false-negative, most likely because these were small (0.7 cm mean size) lymph node metastases, the group explained. The ROC curve had an area of 0.85.
"We found that SUVs increased with the size of axillary metastases and that there may be a relationship with the size of the primary tumor," the authors wrote. "Larger axillary metastases were more likely to be PET-positive."
At an SUV threshold of 2.3, PET turned in a specificity of 100% and a sensitivity of 60%, which suggested that the clinical benefit of PET for noninvasive staging of axilla is in its specificity, the authors stated in their conclusion. In comparison, MR studies in this setting have shown specificities ranging from 56% to 100%. Ultrasound-guided procedures have also turned in 100% specificity but are limited to patients with abnormal lymph nodes, they noted.
The authors cautioned that PET SUVs can vary by as much as 15%, depending on acquisition protocol and other technical factors. They recommended that each PET center rely on its own reproducible reference values before using the modality in this clinical setting.
In a discussion of this paper, Dr. Armando Giuliano, director of the Joyce Eisenberg Keefer Breast Center in Santa Monica, CA, asked how reliable the PET exam was and how the information could be used by an operating surgeon.
"The answer is that (PET) is not a perfect test, but by quantifying the activity, it can become a more accurate test," replied Dr. Edward Phillips, one of Chung's co-authors. "It is more useful in its specificity than its sensitivity. There were patients who had PET activity in the axilla, and the surgeon assumed positive nodes and proceeded right to AND."
In an e-mail to AuntMinnie.com, Waxman broke down some of the costs associated with PET in this setting. "The radiopharmaceutical is approximately $250 per dose ... maintenance, repairs, utilities, space etc., will result in a $1,200 to $2,000 technical fee without a professional component. Reimbursement for a global billing is now about $1400," he wrote.
Waxman and Phillips also told AuntMinnie.com that they will continue with their research in breast cancer, using PET/CT, which may help identify smaller tumors.
By Shalmali Pal
AuntMinnie.com staff writer
August 21, 2006
Related Reading
Breast cancer-involved sentinel nodes often contain micrometastases, August 15, 2006
SLN procedure in pregnant breast cancer patients leads to negligible fetal dose, August 14, 2006
Risk factors for ipsilateral breast tumor recurrence identified, February 1, 2006
Dual-time-point breast PET increases diagnostic accuracy, December 2, 2005
Copyright © 2006 AuntMinnie.com