Electron beam computed tomography (EBCT) has been found to be a reliable method of evaluating coronary luminal stenosis, given adequate image quality. Yet image quality is anything but given, considering that poor spatial resolution and significant heart-motion artifacts have often limited the usefulness of this promising technique.
Inconsistent image quality is what led researchers from the Harbor-UCLA Medical Center and St. John's Cardiovascular Research Center in Torrance, CA, to look for new ways to optimize image acquisition.
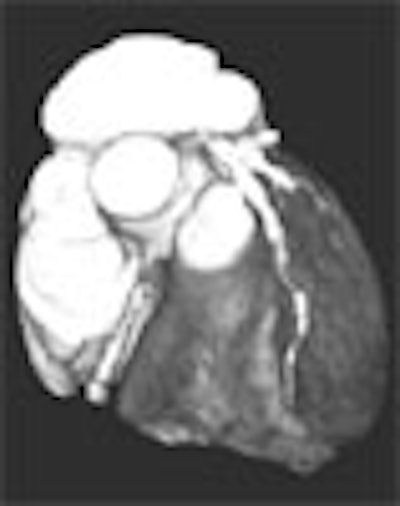
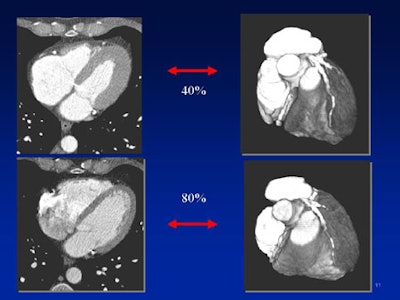
In a departure from previous studies, the team found that it acquired its sharpest images at the end of the systolic phase, rather than mid-way through it. Dr. Bin Lu presented the group's findings at the 2001 American Roentgen Ray Society meeting in Seattle.
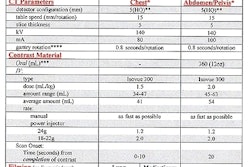
The team performed the electron beam angiography procedure on a dedicated electron beam tomography scanner, (C-150LXP, Imatron, South San Francisco, CA), Lu said. The procedure combines three protocols, including calcium screening, flow study, and CT angiography.
Images were acquired in 100 consecutive patients using 2-mm slice thickness, breathholding of 31-57 seconds, and ECG triggering at R-R intervals set variously at 80% and 40%. Fifty-five slices were acquired for each patient using a voxel size of 0.34 0.34 x 2 mm3 (7 line pairs per centimeter), and following injection of 120-160 ml of iopamidol 370 contrast at 4ml/sec. Three-dimensional reconstruction was performed using a volume-rendering technique (Imatron software version 12.34).
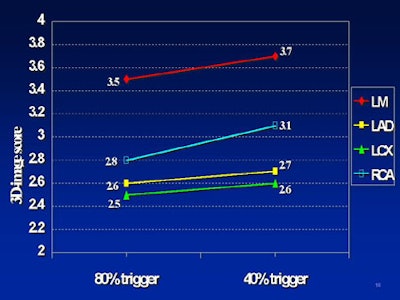
In the 2-D images, the contrast-to-noise ratio was used to evaluate image quality. "In the 3-D images we used a five-point scale," Lu said. "Zero means that no calcium was visualized; 1 means poor image quality, nondiagnostic; 2 means average image quality, diagnostic; 3 means very good image quality, diagnostic; and 4 means excellent image quality, diagnostic."
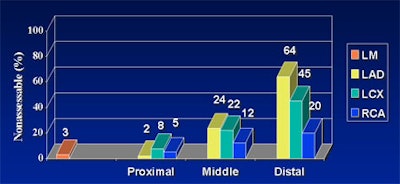
According to the results, the technique failed completely in 7% of patients due to image artifacts, Lu said. Image scores were highest in the left main coronary artery (LM) at 3.6, followed by the right coronary artery (RCA) at 3.0, the left anterior descending (LAD) at 2.7, and the left circumflex (LCX) coronary artery at 2.6 (p<0.001).
 |
 |
 |
More than 80% of the coronary segments were analyzable using the technique, Lu said, with image quality decreasing progressively from LM to RCA, and LAD to LCX. Scanning technique, optimal ECG triggering, and patient control were all important factors affecting image quality, he said.
"We can get higher resolution by using 1.5-mm slices. This is very important. I recommend that you use 40% rather than 80% R-R interval to reduce coronary motion artifacts. It's better to use high-density contrast, and a higher reduction rate," he said.
The study's most important finding was that heart motion reaches its lowest point at the end of systole (at approximately the 40% R-R interval or T-wave) rather than at mid-diastole (approximately an 80% R-R interval before the P wave), Lu told AuntMinnie.com. Imaging at 40% R-R interval can go a long way toward reducing artifacts associated with coronary artery motion, he said.
In a later ARRS presentation, Lu discussed the results of a second study built on the findings of the first. Here the team sought to pinpoint optimal ECG triggering intervals by acquiring CT data throughout the cardiac cycle at 58-msec intervals. In 70 patients they found that coronary artery motion varies significantly during the cardiac cycle, and that it increases with increasing heart rates, according to the study abstract.
For patients with heart rates < 70 bpm, 71-100 bpm, and > 100 bpm, the least motion of the right coronary artery occurred at 60-80%, 30-50%, and 40-60% R-R intervals, respectively. The optimal ECG trigger time was found at an R-R interval of approximately 35% in patients with heart rates < 70 bpm; 50% at 71-100 bpm; and 55% in patients with heart rates > 100 bpm.
By Eric BarnesAuntMinnie.com staff writer
June 13, 2001
Related Reading
EBCT deemed accurate for diagnosis of obstructive CAD, April 4, 2001
Electron-beam CT detects asymptomatic CAD, July 26, 2000
EBCT outperforms stress testing in detecting coronary artery disease, July 4, 2000
Click here to post your comments about this story. Please include the headline of the article in your message.
Copyright © 2001 AuntMinnie.com