The low completion rate for follow-up recommendations on incidental findings detected on imaging exams has long been a thorny challenge in radiology. In an effort to tackle this problem and increase the percentage of patients who adhere to follow-up imaging recommendations, researchers have identified the factors that influence noncompletion rates and have turned to techniques such as AI and commercial software applications to help close the loop.
For example, a group from the University of Rochester in Rochester, NY, recently shared results from using their Backstop recommendation tracking system to directly notify patients of incidental imaging findings that need to be acted on.
 Ryan Loftus, MD, of NYU Langone Medical Center.
Ryan Loftus, MD, of NYU Langone Medical Center.
"Anywhere from 28 to 77% of incidental findings actually get followed up on," explained corresponding author Ryan Loftus, MD, in an interview with AuntMinnie.com. "So if you look at the middle, that's about 50% or half of all findings don't get followed up on, and these are cases where you can catch a disease in its early stages."
In their study published October 9 in the Journal of the American College of Radiology, the researchers sought to assess the efficacy of Act 112, Pennsylvania's Patient Test Results Information Act that became effective December 23, 2018. Loftus, now an NYU Langone Medical Center neuroradiology fellow, and colleagues found that early notification in compliance with this law may not have a positive impact on improving rates of follow-up.
 Ben Wandtke, MD, of the University of Rochester.
Ben Wandtke, MD, of the University of Rochester.
Laws of this sort may be flawed on many levels, according to Ben Wandtke, MD, who also participated in the Backstop study. Wandtke is chief of diagnostic imaging at FF Thompson Hospital in Upstate New York and also an associate professor in the department of imaging sciences at the University of Rochester Medical Center.
"There are a lot of issues with the way the legislation was written," Wandtke told AuntMinnie.com. "If it were replicated to other states or nationwide, it would be a huge disservice to the practice of incidental findings tracking."
There's a widespread problem with incidental findings, Wandtke continued.
"Every health system is dealing with them," Wandtke said. "Follow-up is extremely variable and inconsistent, so there are opportunities to add value. The problem is it's been challenging to identify standard metrics for performance across sites. There's no standard benchmark for performance, and people are just getting into recommendation follow-up and tracking where they're starting to gather data about their own follow-up rates in their organizations."
Wandtke recommends that sites use the American College of Radiology (ACR) Learning Network if they are interested in starting an incidental findings-tracking initiative.
A prevalent issue
Beyond tracking and managing the follow-ups themselves, weighing the pros and cons of recommending and ordering follow-up exams for incidental findings also confronts healthcare professionals and patients along the continuum of care.
In a clinical perspective article published in January 2023 in the American Journal of Roentgenology, Matthew Davenport, MD, of Michigan Medicine in Ann Arbor, MI, noted that approximately 20%-40% of CT examinations and 15%-30% of all diagnostic imaging performed on low-risk patients contained at least one incidental finding.
“Detection of some incidental findings can improve health, but most do not,” Davenport wrote. This is especially true for many patients who are diagnosed with incidental, early-stage cancer (e.g., grade 1 prostate cancer, cystic kidney cancer, and micropapillary thyroid cancer), he said.
For example, Davenport noted that while the incidence of thyroid cancer approximately tripled in the U.S. between 1975 and 2009 and led to healthcare expenditures in the billions, the increase was “nearly entirely explained by increased diagnosis of asymptomatic, indolent papillary thyroid cancer."
Low-value care?
Was there an overdiagnosis epidemic in this case? Davenport suggested there were “strong parallels” to the results of intentionally screening low-risk patients with whole-body scans, a practice that has been discouraged by the ACR and, in the case of whole-body CT, not recommended by the U.S. Food and Drug Administration (FDA), Davenport stated, “owing to the low probability of identifying important disease and the high probability of downstream, low-value care.”
In a recent presentation, "What to do about incidentalomas on imaging," Hailey Choi, MD, of the University of California, San Francisco, identified thyroid nodules, adrenal nodules, pancreatic cysts, liver lesions, kidney lesions, and ovarian lesions as commonly encountered, the management of all depending on different individual characteristics, risk factors, and recommendations for surveillance, depending on the context.
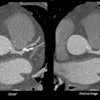
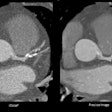
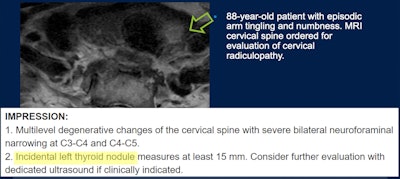 Incidental imaging finding. Image courtesy of Hailey Choi, MD, of the University of California, San Francisco.
Incidental imaging finding. Image courtesy of Hailey Choi, MD, of the University of California, San Francisco.
Toward high-value care, Sucharita Kher, MD, vice chair for clinical operations and quality in the Department of Medicine at Tufts University School of Medicine in Boston, published a letter in late August in JAMA Internal Medicine that emphasized the need to build "systems that allow separating actionable radiological findings from incidental findings and integrate clinical context into this process to allow meaningful clinical outcomes."
Kher, a lung and intensive care unit physician at Tufts Medical Center, drew on data from the National Lung Screening Trial. In cases where the low-dose CT screening exam produced significant incidental findings, 89% of these were considered to be reportable to the clinician. As screening programs become more widely used, more incidental findings will add to the clinical burden, wrote Kher and colleagues in the JAMA Internal Medicine letter.
Some also say that future screening trials, for example, should standardize reporting of significant incidental findings. The ACR and the American College of Emergency Physicians also recently published recommendations on handling incidental findings detected in an emergency room setting.
Managing, tracking, and completing
Hospitals, health systems, referring providers, and patients all have unique perspectives on follow-up imaging recommendations in relation to incidental findings. In response to the issue, an ACR-led initiative developed novel quality measures intended to improve communication and drive increased completion rates for radiology follow-up recommendations. Lung nodules represent about half of all imaging follow-up recommendations, according to the ACR.
The ACR effort honed in on nonemergent actionable incidental findings and overall cancer diagnosis with the goal of enhancing outpatient imaging efficiency, among other drivers. In July 2022, the ACR team published a quality measure set that provides a radiology follow-up recommendation tracking process map.
“Out of many important outcomes that could be measured, detection of cancer is likely the most impactful,” the authors wrote.
Among the takeaway points, the actionable incidental findings ACR measure set fosters a systems approach to closing patient safety gaps, such as missed cancer diagnoses, that may result from incomplete recommended follow-up.
"We've taken some of those metrics which were proposed by experts in the field and put them into practice and tested those with cohorts of individual organizations to see if they work in the real world," said Wandtke, who served as a physician lead for the ACR's Recommendations Follow-Up Improvement Collaborative dealing with incidental lung nodule follow-up. "It's taken some modification, but we continue to learn about how to measure value in performance around incidental findings tracking. And we're getting a lot closer. The National Quality Forum was addressing this as part of its diagnostic excellence campaign, and we're working with the Gordon and Betty Moore Foundation to really hone in on getting some metrics that will eventually be able to be used in registries and shared with national benchmarks ... to drive participation and improvement broadly across the country."
Meaningful patient connections
 Hailey Choi, MD, of University of California, San Francisco.
Hailey Choi, MD, of University of California, San Francisco.
Patients can be an advocate for themselves, Choi said.
"The patient and the referring provider need to take ownership in balancing the risks or the benefits of pursuing [incidental] findings," Choi said. "It has to be a shared decision.”
Choi added the importance of radiology-specialty knowledge in decision-making.
With management and tracking a key piece to ensuring closing care gaps and connecting follow-up recommendations to completion rates, some hospital and health system leaders may be deciding where and how to integrate new tools for provider and patient engagement. These systems will have different capabilities, such as the ability to share medical images and radiology reports, and may enable patients and care teams to proactively manage follow-up care.
Commercial software applications such as PocketHealth's Follow-Up Navigator feature, for example, can help patients manage their incidental follow-up recommendations themselves. And notification and management systems can improve follow-up of incidental imaging findings in emergency department patients.
AI may also have a role to play, such as in helping to triage cases of incidental pulmonary embolism, identify incidental lung nodules on CT reports, and track follow-up on recommendations for incidental lung nodules.