Percutaneous Transthoracic Needle Biopsy:
Technique:
Prior to performing the procedure, patient consent must be obtained. As part of the preliminary work-up prior to the procedure, patients should have a prothrombin time (PT) and platelet count performed within two weeks of the procedure. Anticoagulation and antiplatelet medications (nonsteroidal anti-inflammatory agents) should ideally be discontinued for 7 days. Patients with a single lung (contralateral pneumonectomy) are not generally considered candidates for percutaneous biopsy procedures [Society of Thoracic Radiology Annual Meeting Syllabus 1997; 1-6], although other authors suggest that biopsy of such patients can be performed, although at extremely high risk [12]. Some relative contraindications to transthoracic needle biopsy include an inability of the patient to cooperate (ie: cannot hold their breath or cannot be positioned for the procedure), underlying coagulopathy (PT > 15 sec, international normalized ratio > 1.3, or platelet count below 50,000/cm3), severe COPD (ie: patients who could not tolerate even a small pneumothorax), patient on mechanical ventilation (increases risk for pneumothorax and brochovenous fistula [8]), bullae in the vicinity of the the lesion to be biopsied, a vascular lesion (AVM or aneurysm), and pulmonary artery hypertension [1]. Aspirin use or chronic renal failure can cause platelet dysfunction not reflected in clotting profiles. Some authors [8] consider the previously described conditions to be contraindications to transthoracic biopsy- individual physicians should use sound clinical judgment and discuss the case with the appropriate specialists when making decisions regarding complicated patients.
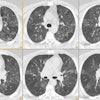
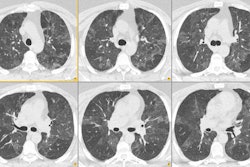
An intravenous line, blood pressure monitor, electrocardiogram leads, and an oxygen saturation monitor should be placed. The biopsy room should be equiped with oxygen, suction, oral and nasal airways, an Ambu-bag (Ambu International, Glostrup, Denmark), a Pleur-evac device (Atrium Medical, Hudson, NH), and a crash cart. After lesion localization, the biopsy needle can be introduced alone, or as a coaxial system. The needle should be passed over the rib (not under) to avoid the neurovascular bundle. Fissures should be avoided because their transgression leads to three visceral pleural punctures rather than one. The use of thin (1-2 mm) localizing images may be very helpful in detecting blebs not seen on thicker section images, particularly in patients with underlying emphysema [8]. Specimens should be obtained during suspended respiration. Cytopathology support during the procedure is essential. In addition to aspiration samples, some centers perform core biopsies cutting needle.
Results:
Percutaneous needle biopsy can be of tremendous value in patient diagnosis. With the use of 20 to 22 gauge aspiration needles and expert cytopathology, sensitivities of 90 to 95% can be expected in the diagnosis of primary intrathoracic malignancy. The ability to distinguish non-small cell from small cell carcinoma approaches 100%. The sensitivity for metastatic disease is between 85-90%. The accuracy of percutaneous biopsy, however, is affected by the size of the lesion, and decreasing accuracy is found to be associated with smaller lesions. Unfortunately, reliability in the diagnosis of benign lesions is not at high with a very variable yield of only 16 to 68% [1]. Often times, a core biopsy will be necessary to confirm that a lesion is benign. An automatic biopsy device with a short throw (1 cm) can significantly increase the diagnostic accuracy for benign lesions, while maintaining acceptable complication rates [2,10,11]. Up to 76% of benign lesions can be accurately identified with the use of a core specimen [10]. In the diagnosis of lymphoma, core biopsy specimens can provide sufficient diagnostic material to guide therapy in 60 to 95% of cases. Unfortunately, the likelyhood for an accurate diagnosis decreases with decreasing lesion size, even with the use of a automatic biopsy device [15]. Cutting guns should never be used in a chronically infected cavity or in regions of bronchiectasis that might be associated with substantial bronchial artery hypetrophy as there is an increased risk for hemorrhage [8].
Because of the low predictive value of a negative biopsy, one may ask does transthoracic needle biopsy ready aid in the management of patient's with solitary pulmonary nodules? It would seem that both patients with biopsies positive for malignancy and those which are negative will still require thoracotomy. Presently, there is not an answer to this question. For suspicious nodules, video assisted thoracoscopic excision can be used for complete removal of the nodule if it is in an accessible location. Tumor seeding along the incisional tract has been reported, and specimens suspected of being malignant should be removed in some type of receptacle [3].
Percutaneous needle aspiration may also be of benefit in the diagnosis of pulmonary infection in immunocompromised patients [14].
Complications:
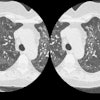
1. Pneumothorax: The incidence of pneumothorax following CT guided transthoracic needle biopsy is generally reported to be between 20 to 30% and is felt to be somewhat higher than the incidence of pneumothorax following fluoroscopic guided biopsy. Most pneumothoraces occur during or within the first hour after biopsy. Only about 2% of pneumothoraces will first appear on four hour post-procedure films. Factors which are associated with an increased risk of pneumothorax include emphysematous changes within the lungs, coughing or breathing during the procedure, increased lesion depth (when traversing aerated lung or crossing fissures), smaller lesion size, multiple pleural punctures, using cutting needles or biopsy guns to obtain core biopsies, prone or lateral patient positioning [12,17], shallow pleural puncture (especially under 50 degrees) [17], and positive pressure ventilation. The use of a coaxial technique permits multiple needle passes from a single pleural puncture. The use of spring loaded biopsy guns should be reserved for large lesions with a diameter exceeding the throw of the needle (usually 20-23 mm) or for those which have a broad pleural attachment. Whether to treat the pneumothorax with a chest tube depends on the patients pulmonary reserve, if the patient is symptomatic (dyspnic), or whether the pneumothorax is enlarging over time. Chest tube drainage of post-procedure pneumothorax is required for between 2% to 14% of cases [4]. The severity of the pneumothorax and the need for chest tube placement appear to be correlated with the severity of underlying obstructive airway disease (emphysema) [5,13]. The majority of pneumothoraces which require chest tube drainage are identified immediately following the procedure [18].
In an attempt to reduce the prevalence of pneumothorax following the procedure several maneuvers have been suggested. Positioning the patient so that the biopsy side is in the dependent position is perhaps the most successful. It is postulated that this maneuver reduces both alveolar size and the differential of alveolar and pleural pressure. These changes favor the development of dependent atelectasis and close approximation of the parietal and visceral pleura. The administration of oxygen (100% at 2-3 L/min) to patients before, during, and following the procedure may also be useful. The theoretic basis for this is that should a pneumothorax develop while the patient is breathing high concentrations of oxygen, the air in the pleural space would also be oxygen rich. A pneumothorax will decrease more rapidly in this setting since oxygen is resorbed into blood faster than air. Aspiration of large immediate post-procedure pneumothoraces using a standard 18 g IV catheter may decrease the need for chest tube placement. In one study of patients with large post-procedure pneumothoraces, immediate aspiration of the air avoided the need for chest tube placement in 70% of these patients [6]. Patients who develop clinically important pneumothoraces have also been managed as outpatients with short-term small caliber chest tubes [7]. Plugging the biopsy tract with autologous blood clot has been advocated by some authors to decrease the risk of pneumothorax, although results are variable [16].
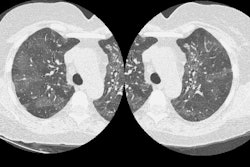
2. Hemorrhage: The incidence of hemorrhage following transthoracic biopsy ranges from 1 to 10%- it is the second most common complication of transthoracic biopsy. The use of a biopsy gun is associated with an increased risk for hemorrhage [8,11]. Hemorrhage is almost always self-limiting [1]. The likelihood of hemorrhage is greater for vascular lesions (such as vascular metastases or chronic inflammatory cavities [due to enlarged bronchial arteries]), patients with an underlying bleeding diathesis (thrombocytopenia, aspirin use), patients with pulmonary arterial or venous hypertension, and with the use of larger cutting needles [12]. Patients with hemorrhage should be placed biopsy side down to decrease the risk of blood being carrying into the opposite lung. During parasternal biopsy procedures, care should be taken to avoid the internal mammary vessels which lie about 1.25 cm lateral to the lateral margin of the sternum.
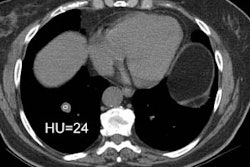
3. Systemic air embolization: This is a very rare complication of the procedure. Air embolism most likely occurs due to air entering the pulmonary vein either directly from the needle open to the atmosphere or from a broncho- or alveolovenous fistula induced during placement of the needle. Factors which increase airway pressure result in an increased risk for air embolism including coughing, the deep inspiration which precedes coughing, and positive pressure ventilation. Biopsy guns may also increase the risk for air embolism [8,12]. Complications of air embolism include myocardial infarction, stroke, or death. As little as 0.5 ml of air is sufficient to induce coronary artery ischemia and fatal arrhythmias. Treatment consists of placing the patient in a left lateral decubitus position (to prevent air within the left atrium from embolizing systemically) or Trendelenberg position (to keep air out of the cerebral circulation). Ventilatory support with 100% oxygen should be administered to promote resorption of air bubbles. Transfer to a hyerbaric chamber may be necessary. [1]
4. Malignant seeding of the biopsy tract: Although seeding may occur, it is an extremely rare complication (0.012%). The risk malignant seeding of the biopsy track is random- no definite risk factors have been described [9].
5. Death: The mortality rate from transthoracic needle biopsy is 0.02% [1]
Post-biopsy Management:
Some centers obtain post-biopsy chest radiographs immediately following the procedure, while others delay this exam for one hour to avoid straining associated with rising from a recumbent to a seated or standing position. Selected CT images following the procedure can also be used to evaluate for the presence of a pneumothorax. Patients should be monitored with vital signs, breath sounds, and oxygen saturations every 15 minutes for one hour and every 30 minutes thereafter. The biopsy site should be placed in a dependent position following withdrawal of the biopsy needle. This maneuver decreases alveolar volume adjacent to the puncture site, uses the weight of the lung to help tamponade the puncture, and raises intrapleural pressure thereby decreasing the amount of air leak. An additional benefit of this position is the prevention of transbronchial spread of hemorrhage that may complicate the procedure. The use of a blood patch has been described, but has not been demonstrated to be of significant value. Patients should remain in the biopsy site dependent position for at least 2 hours. If patients that have no pneumothorax following the procedure and at 4 hours post biopsy can be discharged home. Patients with only a small pneumothorax identified on delayed chest radiographs can probably be discharged safely [18]. Patients should be instructed to avoid straining and all but mild physical exertion until the following day. Patients should spend the night following the procedure with a family member of friend [12]. Patients should be instructed to procede immediately to an emergency room for any pleuritic chest pain, hemoptysis (of more than a teaspoon of fresh blood), or shortness of breath. [1,12]
If a small or asymptomatic pneumothorax is present post-procedure CXR's should be obtained at 2 and 4 hours. If the pneumothorax remains stable and the patient remains asymptomatic, they may be released. If the pneumothorax is enlarging (15 to 35% pneumothorax- depending on the patients respiratory status) or becomes symptomatic, an 8 french catheter with a hollow inner trocar should be placed in the lung apex over the second intercostal space in the midclavicular line. The air in the pleural space should be aspirated and the catheter attached to a Heimlich valve or Pleurevac system. Most pneumothoraces requiring chest tube drainage are detected within one hour of the biopsy. [1]
REFERENCES:
(1) J Thorac Imag 1997; Klein JS, et al. Transthoracic needle biopsy: An overview. 12: 232-249
(3) Ann Thorac Surg 1995 Jan;59(1):42-45
(5) Radiology 1996; 198: p.371-375
(6) Radiology 1996; 200: 695-697
(7) Radiology 1997; 205: 249-252
(8) J Thorac Imag 1997;12: 259-271
(9) J Thorac Imag 1998; 13: 2-6
(11) Radiology 1998; Lucidarme O, et al. Intrapulmonary lesions: Percutaneous automated biopsy with a detachable, 18-gauge, coaxial cutting needle. 207: 759-765
(12) Radiology 1998; Moore EH. Technical aspects of needle aspiration lung biopsy: A personal perspective. 208: 303-318 (No abstract available)
(13) AJR 1999; Laurent F, et al. Pneumothoraces and chest tube placement after CT-guided transthoracic lung biopsy using a coaxial technique: Incidence and risk factors. 172: 1049-1053
(14) AJR 2000; Hwang SS, et al. The value of CT-guided percutaneous needle aspiration in immunocompromised patients with suspected pulmonary infection. 175: 235-238
(15) AJR 2000; Tsukada H, et al. Diagnostic accuracy of CT-guided automated needle biopsy of lung nodules. 175: 239-243
(16) Radiology 2000; Lang EK, et al. Autologous blood clot seal to prevent penumothorax at CT-guided lung biopsy. 216: 93-96
(17) Radiology 2001; Ko JP, et al. Factors influencing pneumothorax rate at lung biopsy: Are dwell time and angle of pleural puncture contributing factors? 218: 491-96
(18) Radiology 2001; Dennie CJ, et al. Transthoracic needle biospy of the lung: Results of early discharge in 506 outpatients. 219: 247-251