Over the past 30 years, CT technology has rapidly evolved, and it is now mature. So what are its next frontiers? Further automation and better interventional support, according to a July 13 presentation by Dr. Mathias Prokop, PhD, delivered at the ECR in Vienna.
Prokop, of Radboud University Medical Center, Nijmegen, the Netherlands, reviewed predictions about CT he put forth at ECR in 2017 and offered a few new ones about where the modality is headed over the next decade.
Back to the future
Five years ago, Prokop highlighted how CT's imaging capability expanded exponentially from about 1985 to 2010, going from two, four, and 16 rows to 64 and now 320 rows.
"This growth has now stopped, and [the technology] is stable," he said. "CT is a mature technique."
During that lecture, Prokop suggested that CT would include ultrahigh-resolution detectors within a few years and photon-counting detectors within five to 10 -- both of which have been realized (in fact, Siemens Healthineers received clearance from the U.S. Food and Drug Administration for a photon-counting device in September of last year).
As the technology stands in 2022, its hardware features ultrahigh-resolution capability, tables that can scan up to 73 cm per second and handle patients up to 600 lb; gantries with 60 cm to 80 cm bores and speeds of less than 0.25 seconds per rotation; tubes of up to 120 kilowatts (kW) with rapid kilovolt (kV) switching, up to 1300 milliampere (mA), and 70 to 150 kV; and standard detectors of 0.5 to 0.25 mm and photon-counting detectors of 0.2 to 0.4 mm; and dedicated scanners for breast and cardiac applications. And CT software is ever more focused on automating exams and reconstructing images.
Why is all this important? Because of the coming ratcheting up of healthcare needs over the next 20 years, Prokop said.
"When I look at the future, I see that we're going to need at least twice as many personnel," he said. "That's probably not possible, so there will be twice as much work per person. [We'll need to address this problem] with the clever use of technology, automating when possible."
New frontiers
So what's next in the field of CT? Existing CT technique needs to be "cleaned up" in the following ways, according to Prokop:
- Making better use of low-dose options
- Boosting resolution through task-optimized detector configurations
- Improving imaging capability through dual-energy/subtraction techniques
- Accomplishing better motion and metal artifact correction
In addition, there are also new CT frontiers that must be explored, from automating as much as possible to further development of motion analysis capability, he said. He offered a short list of CTs cutting edges over the next few decades:
- Automating "almost everything"
- Developing functional capability such as 4D-CT for perfusion/motion/ventilation/adhesion
- Making real-time, low-dose interventional guidance a reality
- Using cameras in and around the scanner for better patient positioning
- Improving contrast injection and dosage -- for example, with a table that weighs the patient and automatically delivers an appropriate injection
- In-room scanning operation, perhaps via a tablet
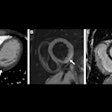
- Expanding CT perfusion capability to cardiac, solid organ, and lung applications (which will require a simple scan protocol, excellent motion correction, and powerful noise suppression, Prokop said)
- Motion analysis capability, such as evaluating ligamental instability in the wrist, patellar instability in the knee, swallowing, and ventilation
The biggest frontier of all, according to Prokop, is developing the use of CT with interventional procedures in order to provide 3D needle guidance, 2D fluoroscopy, and real-time image registration.
"Photon-counting has brought CT to a plateau for the next 10 to 20 years," he concluded. "But a lot of clean-up is needed, and there are quite a few areas we can further develop, with automation and intervention being the most important ones."