Brain changes seen on MR in children treated for central nervous system tumors do not necessarily predict relapse, according to Italian researchers. Nevertheless, the neurological alterations brought on by chemotherapy and radiotherapy need to be watched closely with imaging, and correlated with the patient's clinical and cognitive courses, they stated.
The study, led by Dr. Filippo Spreafico, was conducted at two institutions: the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan and the Istituto Scientifico "Eugenio Medea" in Lecco. The patient population consisted of 49 patients. Of these, 25 had malignant glioma, 16 had medulloblastoma, and eight had supratentorial primitive neuroectodermal tumors (sPNET). The median age at diagnosis was 7.1 years.
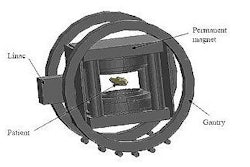
Patients received myeloablative-dose chemotherapy with peripheral blood stem cell rescue (PBSC), both combined with radiotherapy (RT). The latter was scheduled before or after PBSC transplantation and was delivered to a volume defined by T1-weighted gadolinium-enhanced preoperative MR scans.
Medulloblastoma and sPNET patients received hyperfractionated accelerated RT (39 Gy total dose) to the craniospinal axis plus a boost to the posterior fossa or tumor bed. Glioma patients were treated with high-energy photon beams (50-60 Gy total dose).
MR studies included T1-weighted, T2-weighted, and fluid-attenuated inversion-recovery imaging at various intervals over a median of 42 months. "(MRI) lesion-free survival was defined as the probability of remaining without MRI anomalies in the interval between RT (taken as the conventional starting point) and the earliest change detected on MRI studies," the authors wrote (International Journal of Radiation Oncology, Biology, Physics, September 27, 2007).
According to the results, of the 49 children, 37% had therapy-induced lesions at MRI, which were first observed at a median of eight months after radiotherapy. Half of these 18 children had neurologic signs or symptoms judged to be related to the onset of radiologic changes, the group stated.
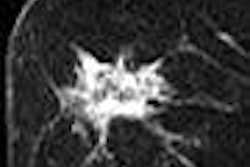
On MR, the therapy-related anomalies were all isointense to gray matter on the T1-weighted images and hyperintense on T2-weighted images. Patterns of enhancement were nodular and curvilinear. The authors reported that the lesions developed mainly in the periventricular white-matter area with some involvement of the overlying cortex. The overwhelming majority of children, 94% of the 18, had multiple lesions.
Of the six kids with malignant glioma and MR lesions, the lesions started to improve 11 and 24 months after onset. Of the dozen medulloblastoma/sPNET patients, six continued to have signs of lesions on MR scans done a little more than a year after onset. In 15 of the 18 patients with follow-up of more than one year, five lesions regressed completely and eight had partial regression.
The MRI lesion-free survival rate for the entire cohort was 74% ± 6% at one year and 57% ± 8% at two years. In a subanalysis of 25 patients (12 with MR lesions and 13 controls without lesions), no significant correlations were found between IQ and MR changes, but this may have been due to the small sample size, the authors stated.
"The available evidence suggests that brain abnormalities are common in early MRI findings in children treated with myeloablative-dose chemotherapy and brain RT.... The more intensive treatment strategies used for high-risk pediatric brain tumors might warrant reconsideration for what is 'normal' or 'abnormal' findings on brain MRI scan," they concluded.
The group noted that several issues still need to be resolved in this treatment paradigm. First, does giving radiation before or after PBSC increase neurotoxicity? Second, was the use of craniosacral radiation the reason that sPNET patients experience cerebrospinal fluid leakage or was it because of the higher number of lumbar punctures?
Finally, "a major challenge in our, and other, experiences was differentiating treatment-induced damage from recurrent tumor, given the therapeutic and prognostic implications," the authors wrote. Pointers to therapy-related MR lesions included location with the periventricular white matter and gadolinium enhancement, they suggested, adding that MR spectroscopy has shown promise as a modality that can separate progressive tumor from treatment-related necrosis.
By Shalmali Pal
AuntMinnie.com staff writer
October 12, 2007
Related Reading
Genetic variation affects low-grade glioma response to temozolomide, May 24, 2007
Radiation increases risk of new CNS tumors in childhood cancer survivors, November 2, 2006
Copyright © 2007 AuntMinnie.com