While mammography remains the most reliable method for detecting breast cancer today, researchers have continued to study new technologies for women with dense breast tissue and those with increased risk of breast cancer. Several studies have shown that mammography has reduced sensitivity in these high-risk women, but MRI has proved to be a costly alternative for breast evaluation.
A team of researchers at the Mayo Clinic used a solid-state scintimammography system to perform what they called molecular breast imaging (MBI) in a population of 48 patients. They said that the technique has comparable sensitivity and specificity to MRI and is four to six times less expensive. Their study was presented at the U.S. Department of Defense's Era of Hope conference in Baltimore last week.
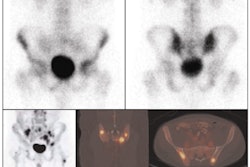
The Mayo Clinic researchers used dual-head prototype gamma cameras -- one developed by Gamma Medica-Ideas of Northridge, CA (LumaGEM), and the other by the Haifa, Israel-based nuclear medicine division of GE Healthcare of Chalfont St. Giles, U.K. -- to detect the preferential uptake of technetium-99m sestamibi in breast disease.
Both gamma cameras are based on digital semiconductor pixilated detectors and differ from another approach to scintimammography, breast-specific gamma imaging (BSGI, Dilon Technologies of Newport News, VA), which utilizes a scintillating crystal technology. A study published in the June issue of Radiology showed that BSGI is as sensitive as MRI for detecting most breast cancers and is more sensitive for ductal carcinoma in situ (DCIS).
Although the Mayo group did not compare their system to the BSGI technology, they said it is more sensitive than performing scintimammography on a whole-body gamma camera.
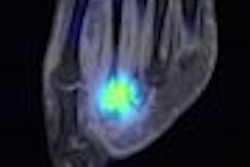
"By using a semiconductor pixilated device we can pick up much smaller tumors than [whole-body] gamma cameras based on scintillating crystal technology -- even those under 5 mm," noted Carrie Beth Hruska, Ph.D., the lead author of the Mayo Clinic study.
The researchers used gamma cameras with dual detectors, one on each side of the breast, to perform their evaluation of each patient. Previous investigations performed at the Mayo Clinic by the team of researchers who did the MBI study have shown that this technique improves breast cancer detection by 10% or more, according to Hruska.
"The images have high spatial resolution, high energy resolution, and good contrast," she said. MBI, in contrast to MRI, also produces only four images that can be interpreted within five minutes by a radiologist, making it more cost-effective than MRI, they believe.
In the Mayo study, 48 patients underwent imaging by both MRI and MBI. The gold standard for comparing sensitivity of MRI and MBI was either tissue pathology or breast status at 15 months of follow-up for those patients who did not undergo biopsy or surgery.
A total of 54 cancers in 32 patients were diagnosed. MRI detected 53 cancers in 31 patients for a sensitivity of 98%, and MBI detected 51 cancers in 30 patients for a sensitivity of 94%. One cancer (a DCIS present in all four quadrants) was not diagnosed with either MRI or MBI and was also occult on mammography and ultrasound. Sixteen patients had negative findings, of which nine were true negative on MRI for a specificity of 56%, and eight were true negative on MBI for a specificity of 50%.
Further diagnostic evaluation was performed in 12 patients due to false-positive MRI findings, prompting nine biopsies of benign areas. MBI studies were false positive in 11 patients, prompting seven biopsies of benign areas.
"We wanted to see if it was possible for MBI to compete with MRI and we were pleasantly surprised by the results," Hruska said. "The problem with MRI is that it is so sophisticated and complex, and the costs associated with using the technology and interpreting images are huge."
The researchers concluded that MBI has a comparable specificity and sensitivity to MRI and may be a cost-effective alternative. They plan a number of follow-up studies, including a prospective study of 120 high-risk patients who will undergo both MRI and MBI. They also are working on using alternative radiotracers in their studies, including one based on angiogenesis, Hruska said.
By Barbara Boughton
AuntMinnie.com contributing writer
July 2, 2008
Related Reading
BSGI sensitive in detecting cancer, study says, May 30, 2008
Breast gamma imaging spots DCIS better than mammo, MR, August 13, 2007
ARRS study: Scintimammography shows high sensitivity in breast cancer detection, May 9, 2007
Molecular breast imaging sensitive for detecting smallest tumors, January 21, 2005
Copyright © 2008 AuntMinnie.com