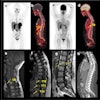
The 2006 RSNA meeting program boasts no less than 27 talks on the role of PET imaging in breast cancer. Topics covered include the modality's accuracy in metastatic breast cancer (education exhibit LL-BR4833), staging locally advanced breast cancer with FDG-PET/CT (scientific poster LL-NM2090-H08), and the efficacy of a hypoxic imaging agent as assessed with microPET (scientific paper SSA23-03).
While the presentations above focus on pretreatment imaging, one education exhibit (LL-BR5200-D) will discuss FDG-PET/CT for post-therapy monitoring. Two published papers out of the U.K. and Australia tackle that same subject. The first used FDG-PET to predict breast cancer's pathologic response to therapy, while the second used the modality for prognostic stratification after high-dose chemotherapy.
Neoadjuvant chemotherapy
A lack of clinical response to neoadjuvant chemotherapy occurs in one-fourth of patients who are treated for primary breast cancer, and about one-third actually achieve a complete pathological response, according to Dr. Gary McDermott from the University of Aberdeen in Scotland.
"FDG-PET may allow identification of patients with poorly responding tumors in the early stages of chemotherapy justifying a revision in the early stages of chemotherapy," the group wrote in Breast Cancer Research and Treatment. McDermott's co-authors are from the Aberdeen Royal Infirmary and Eli Lily in Surrey, U.K. (Breast Cancer Research and Treatment, August 9, 2006).
For this study, 96 female patients with large tumors (T2 > 3 cm) or locally advanced breast cancer (T3 or T4 with any N status) were enrolled. They each underwent six to eight cycles of anthracycline-based chemotherapy, with three weeks off in between cycles. This treatment was followed by breast conservation surgery or mastectomy.
PET images (ECAT EXACT 31, CTI Molecular Imaging/Siemens Medical Solutions, Knoxville, TN) were acquired before chemotherapy, at the end of the first treatment cycle, at the midpoint of the treatment cycle, and at the end point, before surgery. For each scan, 185 MBq of FDG was administered.
In total, FDG-PET images were acquired in 75 locally advanced breast cancer tumors at the end of the first cycle, 58 at the midpoint, and 67 at the end point. Only 30 images were obtained on all four occasions due to missed post-therapy images, the authors explained.
According to the results, only tumors with an initial tumor-to-background ratio (TBR) of greater than five showed a difference between response categories. The average volume for tumors with TBR less than five was 10 ± 3 cm3 versus 42 ± 9 cm3 for those with an average TBR of greater than five.
"For tumors with high pretherapy image contrast, results indicate diagnostic discrimination for chemotherapy response was high; (receiver operator characteristic) areas were 0.83-0.93 and 53%-77% of tumors with a low pathologic response could be positively identified," the authors wrote.
For response discrimination, they found that FDG-PET exams done at the midpoint of therapy identified 77% of the low-responding tumors and 100% of the high-responding tumors.
Minimal changes in tumor response between the midpoint and end point of therapy may be because of a therapy-induced reduction in vascular delivery, the authors suggested, adding that this vascular delivery restriction lowers PET's sensitivity to metabolic changes as chemotherapy progresses.
"Our results suggest that the most prudent time to monitor chemotherapy response using FDG-PET is between the end of the first cycle and the midpoint of chemotherapy, which is a compromise between avoiding the early phase where tumor FDG uptake falls rapidly and minimizing the patient's exposure to toxic chemotherapeutic agents," the group stated.
In addition, FDG-PET monitoring is most likely to be effective in tumors that are about 3 cm in diameter and in metabolically active tumor types such as invasive ductal carcinoma, they added. Finally, they recommended the use of a background-based mean standard uptake value approach because of its sensitivity to tumor image contrast.
High-dose chemotherapy
Unlike neoadjuvant therapy, high-dose chemotherapy (HDC) remains controversial, especially because a survival benefit has yet to be determined, despite high therapeutic response to HDC when paired with autologous bone marrow or stem cell transplantation.
In a previous study, Dr. Rodney Hicks and colleagues from the Peter MacCallum Cancer Centre in Melbourne, Australia, demonstrated that FDG-PET results could predict survival chances in patients treated for non-small cell lung cancer (NSLC). They applied that evaluation strategy to 47 women with metastatic breast cancer. Hicks' co-authors are from the University of Melbourne and the Cancer Center Jen Perrin in Clermont-Ferrand, France.
For this research, patients received a maximum of three consecutive cycles of HDC, supported by autologous stem cell transplantation and filgrastim. The last dose of filgrastim was given at least two weeks before the PET studies to minimize reactive bone marrow changes, which would obscure residual bone disease, the authors explained.
FDG-PET scans were performed one month after the last cycle of HDC (Quest 300-H, GE Healthcare, Chalfont St. Giles, U.K.) with 70-120 MBq of FDG. Ultrasound and CT images were performed before the molecular imaging study. The PET images were read independently of the CT scans, then with the CT scans, although "this was only for correlative purposes and where there was discordance; the PET result was used exclusively," the group wrote (Journal of Clinical Oncology, July 1, 2006, Vol. 24:19, pp. 3026-3031).
A negative PET scan was labeled as complete metabolic response. Therapeutic response was defined as complete, partial response (30% decrease in the sum of the longest diameter of target lesions), progressive (20% increase), and stable disease (no decrease or increase).
According to the results, 72% of the patients were deemed to have a complete metabolic response after the final HDC cycle. In a subgroup that underwent FDG-PET scanning pre- and postautologous stem cell therapy, 68% achieved complete response.
The median survival time was 19 months in an 87 month follow-up period. Not surprisingly, patients with negative FDG-PET results after HDC had significantly longer survival than those with a positive PET scan.
"The FDG-PET result was the most powerful and independent predictive factor of survival. A positive PET scan one month after HDC increases the relative risk of death ... fivefold," the authors stated. "We demonstrated that a single FDG-Pet scan performed one month after HDC is strongly predictive of survival."
At one year, 89% of the patients with a complete metabolic response were alive versus 38% of those who did not achieve a complete metabolic response, they added.
"In the context of (the) controversial role of HDC and autologous stem cell transplantation, our data provide evidence that FDG-PET can identify a subgroup of patients for whom HDC appears to have achieved a relative prolongation of survival. Larger prospective studies are needed to bolster these results," the group stated.
By Shalmali Pal
AuntMinnie.com staff writer
October 30, 2006
Related Reading
Dual-time-point PET spots local, distant breast metastases, September 14, 2006
Preop FDG-PET spots axillary involvement in breast cancer, may obviate biopsy, August 21, 2006
High-dose chemo bests dose-dense conventional therapy for high-risk breast cancer, December 2, 2005
Copyright © 2006 AuntMinnie.com