The conclusion may seem anecdotally obvious to many U.S. radiologists, but new data is confirming a connection between the hot-button issues of malpractice liability and the growth in utilization of diagnostic imaging.
More than 90% of the specialists surveyed in a new study said they had engaged in so-called defensive medicine to shield themselves from the threat of liability, and three-quarters said they did so "often."
When asked about their latest act of defensive medicine, the ordering of unneeded CT, MRI, or x-ray studies was by far the most commonly cited choice.
The study, led by David Studdert of the Harvard School of Public Health in Boston, appears this week in the Journal of the American Medical Association.
"We investigated defensive medical practice within a state that has been significantly affected by the latest escalation of liability costs and surveyed the six specialties that pay the most for liability insurance," the authors said (JAMA, June 1, 2005; Vol. 293:21, pp. 2609-2617).
Specifically, the researchers sent surveys to a random sample of 1,333 physicians in Pennsylvania practicing in the follow specialties: obstetrics/gynecology, general surgery, radiology, emergency medicine, orthopedic surgery, and neurosurgery.
A total of 824 physicians responded to the survey. The vast majority (96%) had spent at least 10 years in practice; their settings included medical groups (39%), hospitals (28%), and solo practices (20%).
A substantial majority of the 824 -- 88% -- had been sued at least once in their career, and 48% had been sued within the previous three years.
More than half of the respondents had gone through the stress of being dropped by a liability insurer in the past 10 years, usually because their carrier had stopped writing policies altogether in Pennsylvania.
The researchers looked at two types of defensive medicine, which they defined overall as "a deviation from sound medical practice that is induced primarily by a threat of liability."
Some tactics, which the authors called assurance behavior, "involve supplying additional services of marginal or no medical value with the aim of reducing adverse outcomes, deterring patients from filing malpractice claims, or persuading the legal system that the standard of care was met."
Other defensive medicine strategies, called avoidance behavior, had physicians distancing themselves from sources of legal risk. Not surprisingly, the researchers found that radiologists engaged in a few avoidance behaviors.
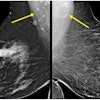
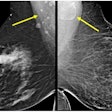
Thirty of the 155 radiologists surveyed said they planned to or had already stopped doing mammography as a way to avoid lawsuits; 24 said they planned to or had stopped performing interventional procedures.
Radiologists were also among those who said they had most recently recommended additional imaging as a defensive practice, although they did so less often than physicians in other specialties.
Among respondents specifying their most recent defensive medicine practice, the ordering of an extra CT, MRI, or x-ray was cited by 63% of the emergency physicians, 41% of the general surgeons, 55% of the orthopedic surgeons, 58% of neurosurgeons, and 36% of radiologists.
Concerns about missing cancer or appendicitis were among the most frequently cited reasons for defensive imaging. Radiologists also reported referring patients with ambiguous mammograms for surgical biopsy and ordering close follow-up with repeat imaging of low-risk abnormalities on chest radiographs.
The physicians who were most likely to practice defensive medicine were those who lacked confidence in their liability coverage or perceived their malpractice premium burden as extreme.
While the authors couldn't quantify the amount of unneeded imaging that might result from defensive medicine, they suggested it could be significant.
"The prevalence of assurance behavior, coupled with the unit of cost procedures typically ordered (e.g., MRIs), lends weight to arguments that the total cost of defensive medicine is substantial," wrote the authors.
The researchers also opined that defensive medical practices would tend to be self-perpetuating.
"The more physicians order tests or perform diagnostic procedures with low predictive values or provide aggressive treatment for low-risk conditions, the more likely such practices are to become the legal standard of care," the authors wrote.
"Reforms to address such 'intensity creep' might include practice guidelines that empower physicians to withhold low-yield tests or force patients to shoulder some of the financial burden, as well as dispute resolution and compensation systems that reduce hindsight bias following injury," the authors suggested. "Professional organizations are well positioned to lead the development and diffusion of such guidelines."
By Tracie L. Thompson
AuntMinnie.com staff writer
May 31, 2005
Related Reading
Bush launches battle to limit malpractice awards, January 6, 2005
Study delineates radiologist risk for malpractice claims, December 17, 2004
AMA sets standards for expert witnesses in medical malpractice cases, December 7, 2004
ACR suspends prominent radiologist for malpractice testimony, October 10, 2004
Court allows suit over radiologist's findings in pre-employment x-ray, August 20, 2004
Copyright © 2005 AuntMinnie.com