CHICAGO - Size really does matter when it comes to predicting high-risk disease in ductal carcinoma in situ (DCIS) of the breast, according to a presentation Sunday at the RSNA meeting. Radiologists from Dublin, Ireland, assessed whether mammographic appearances of DCIS on screening exams could predict patients with high-risk disease.
"Mammography is one of the most sensitive tools for diagnosing DCIS. Mammographically detected calcifications are present in approximately 72% to 90% of cases of DCIS, " presenter Dr. Clare Smith said. "DCIS represents 20% to 30% of all mammographically detected cancer, and 20% to 50% of all cases of DCIS will progress to invasive disease if left untreated."
The purpose of this study was to compare the mammographic and pathological signs of DCIS, compare mammographic features with the pathological grade, and see if these features can be used to predict which patients would benefit from sentinel lymph node mapping, she added.
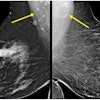
This study included 50,666 screening mammograms from Ireland's BreastCheck program (2001-2003), of which there were 65 cases of pure DCIS diagnosed with core biopsy. Two radiologists reviewed each of these 65 mammograms for lesion size and presence of a mass, as well as presence and type of calcifications.
The Van Nuys classification system was used for size (< 15 mm, 15-40 mm, > 40 mm). Calcifications were divided into two groups, casting and noncasting. The findings on mammography were correlated with histopathological size, grade, presence of micro-invasion, and positive margins of the resected specimen.
Of the 65 patients, "3% presented with a mass on mammography, 68% presented with noncasting calcifications, and 29% with casting calcifications," Smith said. "Seventy-five percent of the cases were high-grade, 20% were intermediate, and 3% were low-grade." The majority of patients, 55%, fell into the 15-40 mm group. A dozen had micro-invasion or invasion.
Overall, there was a poor correlation between the mammographic and pathological size, with 95% limits of agreement between -32.9 and -37.6 mm, Smith said. In each individual size group, "we overestimated the size in less than 15 mm, but we underestimated the size in greater than 40 mm," she explained.
However, the best correlation between radiological and pathological size was in the 15-40 mm group, she said. Lesions with micro-invasion had significantly larger mammographic size (p = 0.002).
"When it came to grade, we found that there was no statistical significance between the different mammographic features, i.e. casting calcifications, noncasting calcifications, or mass. We also found that we could not predict the grade by looking at the mammographic size of the DCIS," Smith said.
The presence of micro-invasion or positive margins at resection did not match with other mammographic features, such as the type of microcalcification or the presence of a mass.
The group concluded that mammographic size, rather than other features, is the most important radiologic determinant in patients with DCIS, especially for tumors between 15-40 mm. "(This) is good because it means that we are not subjecting women to more extensive surgery than is necessary."
Session moderator Dr. David Dershaw asked if Smith's group knew how their pathologists assessed the size of the DCIS, as "it is notoriously difficult for pathologists to measure the size of DCIS." Smith replied that, as far she knew, the pathologists measured from one side to the other, including any gaps.
The outcome of this study reiterates recently published reports. Investigators from the State University of New York in Buffalo found that invasive foci were more likely associated with mammographic calcification size of 11 mm and greater after reviewing 304 cases of breast carcinomas and correlating mammographic features with pathology (American Journal of Roentgenology, December 2003, Vol. 181:6, pp. 1679-1684).
Another group, lead by Dr. Carol Lee from Yale University in New Haven, CT, determined that mammographic and histologic features cannot be used reliably to predict cases that are underestimated with stereotactic core needle biopsy, although the latter is as good as open surgical biopsy for DCIS diagnosis (Radiology, November 2000, Vol. 217:2, pp. 466-470).
By Shalmali Pal
AuntMinnie.com staff writer
November 28, 2004
Related Reading
MRI best for women with heredity risk of breast cancer, September 14, 2004
Early-stage breast cancer survival rates good, March 19, 2004
Study outlines mammographic predictors of invasive carcinomas, January 16, 2004
Copyright © 2004 AuntMinnie.com