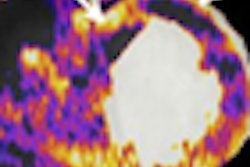
Tighter control of how much radiation is focused on a tumor and how much affects adjacent structures appears to result in less bone marrow toxicity among patients treated with proton beam therapy, when compared with conventional intensity-modulated radiation therapy (IMRT).
Less bone toxicity may allow locally advanced non-small cell lung cancer patients to tolerate a complete chemotherapy regimen, and that may lead to improved outcomes, said Dr. Ritsuko Komaki, professor of radiation oncology at the University of Texas M. D. Anderson Cancer Center in Houston. Komaki presented a paper on the topic earlier this month at the 2008 Chicago Multidisciplinary Symposium in Thoracic Oncology.
"Because proton therapy allows us to control the radiation differently than other types of external-beam radiation therapy, we were hopeful that we could keep radiation away from critical structures, like the bones, to avoid bone marrow toxicity," Komaki said.
The symposium was cosponsored by the American Society for Therapeutic Radiology and Oncology (ASTRO), the American Society of Clinical Oncology (ASCO), the International Association for the Study of Lung Cancer (IASLC), and the University of Chicago.
Komaki and colleagues retrospectively reviewed 142 cases of patients who had undergone radiation therapy at M. D. Anderson for locally advanced non-small cell lung cancer. Of those, 75 patients received chemotherapy plus targeted photon (x-ray) radiation therapy. The remaining 67 patients received chemotherapy and proton beam therapy. The patients in the analysis were treated from January 2003 through June 2008.
All patients in the trial had concurrent chemotherapy and received a 60 Gy radiation dose. Patients were not included in the analysis if they had received other chest radiotherapy. Patients were analyzed for hemoglobin levels, platelets, absolute neutrophils/granulocytes, white blood cell count, and episodes of fatigue.
The demographics of the two groups of patients were similar, although the proton beam therapy patients were older, with a median age of 67 years, compared with a median age of 62 years for the patients treated with x-rays (p = 0.07). Most of the patients in each group had stage III disease, although significantly more were in stage IIIB among the patients receiving x-rays (p = 0.003).
Similar percentages of patients underwent induction chemotherapy and most of the patients were treated with a combination of carboplatin (Paraplatin) and paclitaxel (Taxol).
After a follow-up time of 17 months, researchers found the following:
- Hemoglobin toxicity occurred in 90% of the x-ray patients, compared with 50% of the proton patients (p < 0.001); 12% of proton beam patients experienced toxicities greater than grade 2, compared with 40% of patients treated with x-rays (p < 0.001).
- Platelet toxicity occurred among 33% of the proton beam patients, compared with 48% of the x-ray patients (p = 0.014). There were no differences in patients experiencing greater than grade 2 toxicity.
- Neutrophil toxicity was observed in 18% of proton beam patients, compared with 51% of patients getting x-ray radiation (p = 0.007). About 15% of proton beam patients experienced a greater than grade 2 toxicity, compared with 46% of patients treated with x-rays (p < 0.001).
- White blood cell toxicity was seen in 65% of proton beam patients, compared with 85% of x-ray patients (p < 0.001), and greater than grade 2 toxicities were seen in about 25% of proton beam patients, compared with 79% of x-ray patients (p < 0.001).
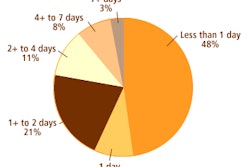
- About 50% of proton beam patients experienced fatigue, compared with approximately 85% of x-ray patients (p = 0.002); about 29% of proton beam patients experienced greater than grade 2 fatigue, compared with 60% of x-ray patients.
In commenting on the trial in a press briefing, Dr. Jeffrey Bradley, associate professor of radiation oncology at the Washington University School of Medicine in St. Louis, noted that "because there is limited use of proton beam therapy, we have very few clinical trials to show how the treatment affects outcomes.
"While this study does show less bone marrow toxicity, it doesn't tell us the clinical outcomes. One could speculate that less toxicity will result in greater completion of chemotherapy regimens, and greater completion of those regimens could result in improved long-term outcomes, but that is two leaps."
He also noted that cyclotrons required to produce proton beam radiation are available at U.S. sites including Harvard University in Boston; M. D. Anderson Cancer Center; Loma Linda University in Loma Linda, CA; and the Lawrence Livermore National Laboratory in Livermore, CA.
By Edward Susman
AuntMinnie.com contributing writer
November 24, 2008
Related Reading
Proton therapy shows promise in treating chondrosarcoma, September 29, 2008
Proton therapy lowers chance of second malignancy, September 23, 2008
Michigan healthcare systems form proton beam partnership, June 3, 2008
Cell survival offers IMRT insight on 'bystander effect,' November 23, 2007
Proton beam therapy effective in controlling hepatic tumors, August 17, 2006
Copyright © 2008 AuntMinnie.com