Already plagued by low reimbursement rates in the U.S., and international controversy regarding its usefulness, the last thing the breast imaging community needs is more unpleasant news. But a recent survey of future radiologists is delivering just that: Residents in the U.S. and Canada have a less-than-positive attitude toward breast imaging and are not inclined to specialize in the field.
A multi-institutional group, including researchers from the University of California, Los Angeles and the Mallinckrodt Institute of Radiology in St. Louis, queried residents from 203 of 206 accredited U.S. radiology residency programs. Third- and fourth-year residents answered a 20-minute phone survey. All of the residents had completed at least one rotation in breast imaging.
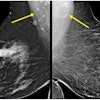
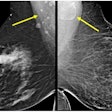
"Our questions addressed training, attitudes about mammography, and interest in performing breast imaging in the future," explained Dr. Lawrence Bassett in a presentation at the 2001 RSNA meeting. "The breast cancer screening population is increasing by an estimated 60%, and is anticipated to increase through the year 2020. This creates a challenge for training programs to provide enough interpreting physicians."
On the whole, the respondents were hardly enthusiastic about breast imaging, reported Bassett, who is the director of the Iris Cantor Center for Breast Imaging at UCLA.
"We asked them to compare breast imaging to other types of examinations, such as CT of the abdomen with contrast excluding the pelvis. For example, we asked them how concerned they were about missing a potentially important finding (in either exam)," he said.
About three-fourths (74%) of the residents said that they were more concerned with missing a finding on mammography. They also replied that they felt more anxiety about making the appropriate recommendation to a referring clinician about the results of a mammogram than they did the CT exam. With regard to practice liability, 93% of those surveyed were more concerned about breast imaging.
The questionnaire also solicited the residents’ opinion on mammography versus all other imaging exams. Again, mammography didn’t gain any points, with 82% of the respondents stating that the stress level associated with breast cancer misdiagnosis was much higher than with other exams. In addition, 93% said they felt that the patient stress level associated with mammography was greater than for other imaging tests.
While 65% of the residents agreed that mammographic exams should be interpreted by a breast imaging subspecialist, 64% said they would not consider doing a fellowship in breast imaging. Moreover, 63% of the residents said they would prefer not to devote a significant portion of their time (25% or more) as a practicing radiologist to mammography.
"The most common reason for not wanting to do breast imaging as a subspecialty was that it is not an interesting field," Bassett said. "The second was fear of lawsuits, the third was that it’s too stressful. Other answers were that the work is too hard and the pay is too low."
On the bright side, institutions are doing their part to promote an interest in breast imaging. Nearly all of the respondents (95%) said they had rotations exclusively in breast imaging. At least eight weeks of mammography training were required by 96% of the healthcare facilities, while 96% had independent breast imaging sections, with a dedicated supervisor who spent at least 50% of his or her time in that section.
The residents also reported that 84% of them always or frequently dictated mammography reports. Under supervision, 36% said they interpreted more than 200 cases a week. Breast ultrasound was performed by 88% of those surveyed, 86% had conducted cyst aspirations, 94% had performed needle localization, and 82% had done ultrasound-guided biopsies.
"In summary, most programs provide at least eight weeks of breast imaging training, including mammography, ultrasound, and interventional procedures. However, attitudes about mammography are often negative," Bassett said. "From this survey, we expect that we will have an increasing shortage of interpreting physicians at both academic and private practices. This may contribute to problems with patients having access to timely, high-quality breast imaging services."
Bassett added that, while this data is disappointing, it is also a challenge that the breast imaging community needs to face, possibly by developing alternative educational programs to keep residents interested, or by offering monetary compensation for those who go into breast imaging.
By Shalmali Pal
AuntMinnie.com staff writer
April 15, 2002
Copyright © 2002 AuntMinnie.com