A connection between chronic low back pain (LBP) and reduced strength, as well as fatigue resistance, in the back muscles has been well documented. In addition, as the muscles degenerate and decrease in size, there is an increase of fat and interstitial tissue. But the question remains as to whether LBP occurs because of these changes or if LBP instigates them. And is there a way to depict fatty degeneration in the early stages of LBP?
A multispecialty group from Switzerland used proton MR spectroscopy (MRS) to prospectively evaluate the fat content of paraspinal muscles in patients with chronic LBP and asymptomatic volunteers. They found that MRS did offer a certain insight into certain muscular components involved in LBP, but didn't necessarily tell the whole story.
"Information about the extent of fatty degeneration of the paraspinal muscles in patients with LBP would be useful for rehabilitation programs," wrote Dr. Bernard Mengiardi from the department of radiology at the Orthopedic University Hospital Balgrist in Zurich. His co-authors are from the hospital's departments of orthopedic surgery and rheumatology, as well as the Institute of Psychology at the University of Bern in Bern, Switzerland (Radiology, September 2006, Vol. 240:3, pp. 786-792).
For this study, 25 consecutive patients with chronic LBP were referred by a clinician for routine diagnostic MR of the lumbar spine. Eleven of the 25 had no compromise of the nerve root; 10 had disk extrusion with no compromise of the nerve root; and one had a disk extrusion with deviation of the nerve root at level L5-S1. Patients self-rated their duration and intensity of pain on a questionnaire. They were matched with a 25-person control group.
MR exams were done on a 1.5-tesla system (Symphony, Siemens Medical Solutions, Erlangen, Germany). The imaging protocol included transverse T2-weighted fast spin-echo images obtained at the L4-5 level and used for voxel positioning. Single-voxel spin-echo proton MRS was performed. On MRS, the percentage fat content was calculated from the areas of fat peak and water peak. The fat content was then graded according to a four-point scale commonly applied to the supraspinatus muscle, with 0 indicating no intramuscular fat and 4 representing more fat than muscle tissue.
According to the MRS results, the mean percentage fat content of the multifidus muscle was 23.6% for the LBP patients and 14.5% for the volunteers. The mean percentage fat content of the longissimus muscle was 29.3% for the LBP patients versus 26% for the control group.
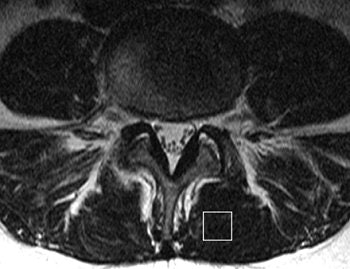 |
| MR image and corresponding MR spectrum of left multifidus muscle in a symptomatic 36-year-old woman. Above, transverse T2-weighted fast spin-echo MR image (4000/122) at left multifidus muscle (square represents voxel location) at L4-5. At semiquantitative analysis, fatty atrophy was graded 0 (no intramuscular fat). Below, MR spectrum (1500/135) reveals elevated lipid peak (L) with 24.7% fat content (mean value of asymptomatic patients, 14.5%). W = water peak. |
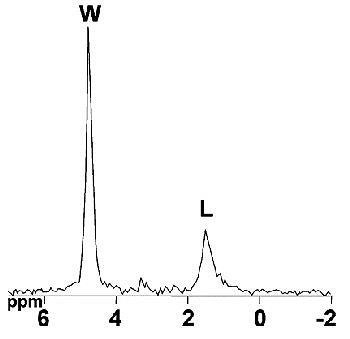 |
| Figures 2a,b. Mengiardi B, "Fat Content of Lumbar Paraspinal Muscles in Patients with Chronic Low Back Pain and in Asymptomatic Volunteers: Quantification with MR Spectroscopy." Radiology 2006; 240:786-792. |
"In our study, patients with chronic LBP had a significantly larger percentage of fat content in the multifidus muscle when compared with that of the asymptomatic volunteers, but there was no significant difference in percentage fat content for the longissimus muscle," the group wrote. In addition, "this significant difference for the multifidus muscle could not be detected with a semiquantitative grading system...."
In 48% of the LBP patients, fatty atrophy of the multifidus muscle was graded as 0. In the volunteer group, 58% had a grade of 0. In the chronic LBP group, the fatty atrophy of the longissimus muscle was graded as 0 in 36% of the cases and 60% of the control group.
In an e-mail to AuntMinnie.com, Mengiardi offered more details on how MRS information can assist the referring physician in planning treatment.
"The radiologist should not only report the disk and end-plate abnormalities, but also the quality of the multifidus muscle as part of the functional unit reading a lumbar spine MRI of an LBP patient," Mengiardi wrote. "In case of a high fat content, the clinician should up-rate the value of physical therapy (with or without surgery) to strengthen the multifidus muscle, thus achieving better long-term results. As our study showed, a visual semiquantitative description of the fat content is inferior compared with MRS."
However, Mengiardi acknowledged that MRS does require additional exam time, so incorporating it into a routine workup will be a slow process. Also, getting clinicians in the habit of relying on MRS information for therapeutic planning will be necessary, but he pointed out that MRS is used quite often in guiding treatment for shoulder and rotator cuff tears.
LBP and healthcare provider
Mengiardi's team did not find a significant correlation between percentage fat content of the back muscles and pain intensity, pain duration, or self-rated disability. In a separate study, a Spanish group asked if there might be a relationship between LBP, disability, MR findings, and the type of healthcare provider.
"Healthcare services in Spain are organized in a national health service (NHS) with compulsory universal coverage. In addition, the private health insurance covers 25% of the population on a voluntary basis," explained Dr. Estanislao Arana and colleagues. "Our work seems to be the first application of an outcome-measures questionnaire for LBP comparing two populations from different healthcare providers" (Skeletal Radiology, June 2006, Vol. 35:9, pp. 641-647).
Arana and several co-authors are from the radiology department at the Clínica Quirón in Valencia, Spain. Other contributors are from the departments of radiology and preventative medicine at the Hospital Universitario Dr. Peset, also in Valencia.
During a four-month period, 278 patients met the inclusion criteria for this study: low back pain without radiculopathy or suspected degenerative disease referred by an orthopedist or neurosurgeon. Exclusion criteria included previous lumbar spine surgery, a history of acute trauma, and MRI contraindications. Of these 278 patients, 109 came from the Spanish NHS while 169 were privately insured.
All patients filled out a six-question disability questionnaire, which addressed such topics as wait time and pain severity, on the day of their MR exam. Disability scores ranged from 2 (no disability) to 28 (severe disability).
MRI was done on two 1.5-tesla units (ACS-Intera NT Gyroscan, Philips Medical Systems, Andover, MA), and the protocol included sagittal T1-weighted spin-echo imaging of the lumbar and lower thoracic spine, sagittal T2-weighted turbo spin-echo imaging, and axial proton density-weighted turbo-spin echo imaging. Two radiologists who were unaware of the patients' disabilities scores reviewed the studies, rating them on a scale of 0-30.
According to the results, patients fell into three categories: LBP, LBP and sciatica, and sciatica only. Subjects with LBP and sciatica had similar MR imaging scores and showed the highest disability scores.
In addition, the authors found that the disability scores were higher in NHS patients versus private ones. The MRI score was significantly higher in the NHS group. Also, the MRI score only correlated with answers to a question on how much the pain interfered with the patient's work. NHS patients showed more days of inactivity and more missed workdays than private patients.
Disk degeneration was unrelated to provider or disability score. Neither population nor disability severity was related to facet degeneration, spinal stenosis, or annular tear. However, degenerative disk disease was more prevalent in private than NHS patients. The time on the waiting list to see the doctor was longer for NHS patients.
"Our work reports increased MR imaging and disability scores in the NHS compared to the privately insured population, despite the fact that the latter group showed slightly higher disk degeneration," the group wrote.
Previous studies have demonstrated that the relationship between self-reported disability, clinical exam, and imaging is not always a simple one in back pain. While a connection was found between MR findings and disability scores in the current study, MR scores only marginally correlated with missed workdays because of pain, the authors added.
Finally, NHS patients reported more disability than private ones. This may be related to previous evidence that showed a higher prevalence of chronic conditions such as LBP in lower socioeconomic groups, who are more likely to avail themselves of NHS services (European Journal of Public Health, March 2004, Vol. 14:1, pp. 63-70).
By Shalmali Pal
AuntMinnie.com staff writer
September 26, 2006
Related Reading
MR overordered by primary physicians for back pain, January 31, 2006
MRI doesn't alter patient care in low back pain, study finds, November 8, 2005
Coding for the back shouldn't be a pain, November 8, 2005
Copyright © 2006 AuntMinnie.com