Perfusion imaging allows CT -- still the primary imaging modality for detecting and staging cancer -- to depict vascular physiology as well as detailed patient anatomy.
In the lungs, kidneys, and other organ systems, perfusion CT's ability to detect the enhancement of microvasculature resulting from tumoral angiogenesis is making it an important tool in oncology imaging. Advances in analysis software in recent years have made it an increasingly popular imaging option for surveillance of cancer patients.
Perfusion has several drawbacks, however, including potentially confounding variations in cardiac output, persistence of beam hardening artifacts in larger patients, degradation of image quality due to patient motion -- and high radiation doses that are under keen scrutiny these days.
Lower x-ray tube potentials, on the other hand, serve to enhance the conspicuity of iodinated contrast, along with reducing patient dose, said researchers from the Mayo Clinic in Rochester, MN, in a presentation at the 2007 RSNA meeting in Chicago. To lower the dose, they reduced the x-ray tube energy (kVp).
"The purpose of our study was to empirically determine the conditions where use of 80 kVp did not degrade CT number accuracy," said lead researcher Dr. Elizabeth McDonald in her presentation.
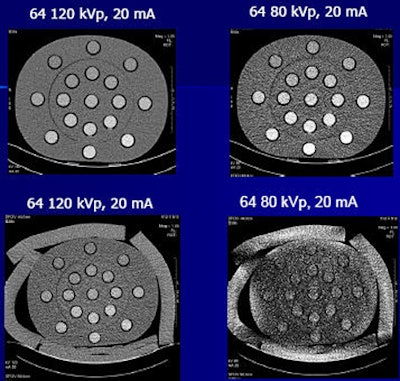
McDonald, Dr. Joel Fletcher, and their colleagues used two anthropomorphic phantoms: one corresponding to larger patients and the other representing a normal adult body habitus. The phantoms included cylinders containing iodine solutions, which were designed to mimic the CT attenuation of enhancing tumor -- that is, 50-210 HU at 120 kVp, McDonald said.
The contrast attenuation differences were created using 17 different saline dilutions of iodinated contrast material to mimic the CT values observed in tumors during perfusion CT.
"Our reference standard was the cylinder measuring 100 HU at 120 kV," McDonald said. An attenuating agent dubbed "Superflab" played the role of fat in the larger phantom.
Both phantoms were scanned in perfusion mode using three scanners: two 16-slice machines and one 64-slice unit at six tube currents ranging from 10-300 mAs, two tube energies (80 and 120 kV), and exposure of one second. The second 16-slice scanner (scanner 16B) was equipped with advanced dose modulation features that reduced the dose at all exposure levels.
There were 16 iodine-filled cylinders in each phantom, and the researchers averaged two mean CT value measurements over each cylinder and for each imaging protocol.
The CT attenuation value measured at each energy setting in the normal-sized phantom at 300 mAs served as the reference attenuation number for each exposure. The researchers determined the noise level at which the perfusion data would no longer be reproducible.
The researchers determined the noise ratio to determine the noise level at which the perfusion data would no longer be reproducible. No scanner yielded predictable attenuation across the board.
At very low exposure levels, the noise level increased dramatically for the larger patient size and 80 kVp data due to the contributions of electronic noise, which is not typically significant at higher exposure levels. Also, the mean CT numbers became inaccurate at the very low exposure values.
 |
| For each scanner there were mAs values that did not reflect truth, and noise levels increased dramatically at low mAs values. |
"For each scanner there are mAs values at which (the mean) CT numbers do not reflect truth," McDonald said. And the accuracy fell in the setting of lower mAs and larger phantom size. "There was also a dose penalty for thinner collimation (at low kVp and large patient sizes) leading to higher doses at 64-slice CT," she said.
At the level of 80 kVp, CT number accuracy was degraded below 50 mAs in the normal-sized phantom and at levels below 100 mAs in the large phantom. When kVp was increased to 120, CT values were accurate for all mAs levels tested in the normal-sized phantom, but in the larger phantom CT attenuation accuracy fell at levels below 50 mAs, she said.
When noise was higher than 40 HU, the reproducibility of CT numbers became unacceptable. As expected, the measured CT attenuation for a given iodine concentration was lower at higher tube currents. As expected, the measured CT attenuation for a given iodine concentration was higher at lower tube potentials (kVps). Additionally, beam hardening in the larger phantom equipped with "Superflab" decreased the observed CT numbers, she said.
In the normal-sized phantom, the iodine signal was at least 50% greater at 80 kVp compared to 120 kVp, McDonald noted. Relative CT values were similar regardless of kVp setting.
McDonald concluded that perfusion CT at 80 kVp may not give accurate results under some conditions, such as in large patients or for pelvic imaging, requiring a higher tube current setting or potential. However, the 80 kVp setting is acceptable in most other circumstances.
"At 80 kVp compared to 120 kVp, the CT number is increased by approximately 60%, noise is increased, and higher mAs values are needed to maintain accuracy for thick patients compared to thin, " McDonald said. "Iodine CT number is decreased by approximately 25% for thick patients compared to thin," she said. "Wider collimation should be used to avoid electronic noise, especially at lower kVp."
Specifically, she said, "We cannot use one generic protocol for all patients for maximum signal to noise. We need technique charts (kVp, mAs, and collimation) for a range of patient sizes." To ensure adequate image quality, "perform a test scan with the selected technique before the perfusion scan to ensure that noise levels are acceptable" (approximately 40 HU or less), McDonald said.
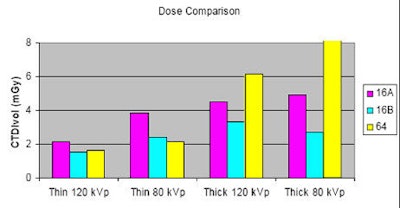 |
| Dose was generally higher in the setting of higher tube current, thinner collimation, and 64-detector-row scanners. |
A tube energy setting of 80 kV may be used in perfusion CT provided that radiologists understand the acceptable imaging requirements for a given patient, the researchers concluded in their abstract.
The exposure and attenuation levels that were deemed acceptable in the study, while not yet optimized for a range of specific patient sizes, are sufficient to do that, McDonald said.
"We can now do a topo scan, and if our noise is above the acceptable value ... we can increase the tube energy," she said.
In response to a question from session moderator Dr. Erik Paulson from Duke University Medical Center in Durham, NC, McDonald said that the measured attenuation values were affected by beam hardening artifact resulting from the layer of simulated adipose tissue, though the magnitude of this effect was unknown.
By Eric Barnes
AuntMinnie.com staff writer
December 10, 2007
Related Reading
256-slice perfusion CT equivalent to SPECT for arteriosclerosis detection, November 13, 2007
Freezing tumors eases cancer pain in study, November 29, 2007
CT enterography answers range of small-bowel questions, May 22, 2007
Distinct CT perfusion parameters help assess HCC, November 29, 2005
Copyright © 2007 AuntMinnie.com