The use of FDG-PET or PET/CT to assess the amount of tumor destruction after radiofrequency ablation (RFA) provides more valuable information than CT alone for the treatment of lung tumors, according to multicenter research presented last week at the American Roentgen Ray Society (ARRS) meeting in Vancouver, British Columbia.
"Usually, CT is used to assess tumor destruction, but CT cannot tell you whether a tumor is still actively metabolizing glucose or is dead in the area of destruction," said Dr. Jennifer Daly of the Newton-Wellesley Hospital in Newton, MA, who presented the group's findings. "It can also be difficult to assess how much of the ablated area is caused by an inflammatory reaction to the procedure," she said.
The study was conducted by researchers from Newton-Wellesley, St. Joseph's Medical Center in Phoenix, the Cleveland Clinic in Ohio, the Dana Farber Cancer Institute and Brigham and Women's Hospital in Boston, and the University of Massachusetts Medical Center in Worcester, MA.
The group assessed 10 lung tumors in 10 patients (seven males and three females with a mean age of 72.5) who had been treated with CT-guided RFA and had PET or PET/CT scans both prior to RFA and following RFA. Each patient had one tumor treated and one patient had the same tumor treated in two sessions, Daly said.
The tumors included seven lung cancer primaries, two metastatic colon cancers, and one metastatic hepatocellular carcinoma with lesion sizes ranging from 3.3 to 34.1 cm2, according to Daly. A comparison was made of the PET or PET/CT studies for each patient to assess for any change in the tumor activity after RFA. The patients had their CT and FDG-PET or PET/CT scans an average of 44.5 days prior to undergoing RFA. After RFA treatment, the patients had their PET scans an average of 76.5 days later.
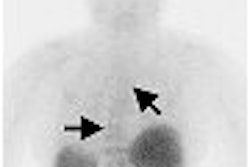
Not surprisingly, all the pre-RFA PET studies showed FDG avidity in the tumors. In seven out of 11 RFA treatments for the 10 patients, the researchers found that the follow-up PET demonstrated persistent rim activity suggestive of a shell of residual neoplasm with a central area of photopenia related to the RFA or postablation recruitment of vessels as an inflammatory response to the injury, Daly said.
Two of the patients showed no activity on the follow-up PET, suggesting complete destruction of any active tumor. One patient had no definite change in the appearance or FDG avidity of the mass compared with the pre-RFA treatment study. One patient had a smaller lesion with the same FDG activity on their follow-up PET; however, the lesion did not have a photopenic center, Daly said. She noted there were procedure-related complications of pneumothorax in four of the patients; two were small and were needle-aspirated, while one resolved itself and required no evacuation.
According to the researchers, without effective follow-up imaging, the radiologist has to gauge how successful RFA treatment for lung cancer was based only on the patient's improvement in reported pain and by what is possibly seen on a postablation CT. With the use of FDG-PET or PET/CT, the amount of tumor destruction after RFA can be determined as long as there are scans taken before and after treatment.
"You don't really know for sure how much active tumor is destroyed unless you compare pre- and post-PET scans," Daly said.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
May 12, 2006
Related Reading
PET/CT is powerful for radiation therapy planning, May 4, 2006
IMRT to 4D radiotherapy rely on QA for accuracy, May 4, 2006
NEMA paper touts imaging's role in oncology, April 6, 2006
Carefully considered radiotherapy stymies endometrial cancer relapse, March 3, 2006
Subcutaneous amifostine feasible during radiotherapy for head and neck cancer, February 28, 2006
Copyright © 2006 AuntMinnie.com