Does computer-aided detection (CAD) software designed for use with chest x-rays have the same potential to help radiologists better detect early lung cancer as mammography CAD has helped the detection of early-stage breast cancer? The answer remains to be determined.
But results of a retrospective study using CAD to analyze chest radiographs containing overlooked indications of lung cancer reveal that CAD software identified nearly half of the tumors missed by radiologists, according to a study from the University of Maryland Medical Center (UMMC) in Baltimore in the July issue of Radiology (2009, Vol. 252:1, pp 273-281).
The study reinforces other published research indicating that CAD technology can help radiologists detect cancerous lesions in chest radiographs of asymptomatic patients. It represents the largest number of patients analyzed to date in a published chest CAD trial, according to principal investigator Dr. Charles S. White, chief of thoracic radiology at the hospital.
Lung cancer is the second most common cancer in both men and women: The American Cancer Society (ACS) estimates that about 219,440 new cases of lung cancer will be diagnosed in 2009. At the same time, diagnosing subtle lung cancer in chest radiography is difficult. After breast cancer, failure to diagnose lung cancer is the second leading cause of malpractice lawsuits against radiologists.
Unlike mammography CAD, chest radiography CAD has not been widely adopted in the U.S. The combination of CAD processing time, the number of false positives generated, low technical and professional reimbursement for chest x-rays, and a high volume of chest x-rays are all factors working against adoption and utilization of the technology.
But for 46 out of 89 patients who were not diagnosed until an average of eight months following a chest radiograph in which subtle lung cancer could have been identified, CAD might have made a difference in treatment protocols, treatment cost, outcomes, and quality of life.
The research
The researchers conducted the study to determine the frequency with which a commercial CAD application (OnGuard version 3.0, Riverain Medical, Miamisburg, OH; pending U.S. Food and Drug Administration [FDA] approval) could identify lung cancers that were overlooked in chest radiographs at the time of interpretation.
They used cancer registries to identify 3,100 patients diagnosed with lung cancer between 1998 and 2006 at UMMC and between 1995 and 2006 at the Baltimore Veterans Affairs Medical Center (BVAMC), all of whose images were contained in each hospital's PACS archives.
Each patient's file was reviewed to identify chest radiographs performed before diagnosis was made, with x-rays collected by either computed or digital radiography. These were reviewed by two experienced thoracic radiologists who had not originally interpreted the exams. For each patient, the earliest radiograph in which an overlooked cancerous nodule could be retrospectively identified with a subsequent CT exam was selected for CAD analysis. The two radiologists assigned a subtlety score to the lesion based on a consensus judgment of lesion conspicuity.
The radiologists identified a total of 114 radiographs (92 posteroanterior and 22 anteroposterior) containing a single overlooked lesion of 89 patients (12 from UMMC and 77 from BVAMC). Ten of the patients had two overlooked radiographs, six patients had three, and one patient had four. Thoracic radiologists had originally interpreted 9% of the exams, thoracic imaging fellows 3%, and general radiologists 88%.
The average lesion size was 1.8 cm, with a range of 0.4 to 5.5 cm. Sixty percent of the overlooked lesions were located in the left lung, and 75% were in the upper lobes. Seventy-one percent of the lesions were peripheral and 29% were central.
The 114 radiographs were processed with the CAD program, as well as 89 radiographs from an identical control group of 89 healthy patients.
The results
The CAD software, trained to detect nodules between 0.9 and 3.0 cm in size, identified missed lesions in 47% of the radiographs representing 52% of the patients. If the software algorithm had been trained to detect lesions up to 4.0 cm, it may have detected 100% of lesions 3.0 to 4.0 mm in size. The CAD software's ability to identify overlooked lesions decreased as the subtlety of each lesion increased.
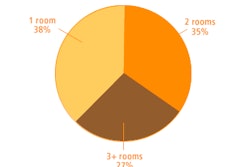
Summary of recommended compression rates
|
The CAD software identified 80% of the lesions in the middle lobe and lingula, compared to 50% of lesions located in the lower lobe and 42% of lesions in the upper lobe.
Zero to five false-positive marks were generated, with an average of 3.9 per image. Citing tolerance of false positives as one of three conditions necessary for chest CAD to gain acceptance among radiologists (the other conditions being sensitivity and workflow integration), the authors noted that this rate was somewhat high. CAD generated an average of 2.4 false positives for the control group's normal chest radiographs.
Newer versions of the OnGuard software generate fewer false positives, according to the company. At the 2008 RSNA meeting, the company demonstrated version 5.0 of the software, which received regulatory approval in Canada and Europe in November 2008.
Future research
No matter how accurate, efficient, or easy to use chest CAD software becomes, the question remains whether radiologists would act upon and accurately diagnose lung nodules identified by CAD software.
White told AuntMinnie.com that UMMC will conduct a study to determine if a mix of residents, fellows, general radiologists, and thoracic radiologists identify subtle lung cancers more accurately with or without the use of CAD. The image set would include a randomized mix of normal chest radiographs along with those containing overlooked cancers on original interpretation.
Readers will be asked to interpret images without CAD, indicating the likelihood of a nodule. After responding, the processed images (using OnGuard version 5.0 software, pending FDA approval) will be displayed and readers will be asked to assess the likelihood of a nodule. The responses to the original image and the CAD-marked image will be analyzed.
A question that will not be answered by this study is whether the FDA will approve new versions of chest CAD software for already approved 510(k) products. To date, no new chest CAD software versions from any company have been approved since 2007.
The FDA held a meeting in March 2008 to discuss the current state of CAD technology and the processes by which CAD should be evaluated for commercial approval in the U.S. A follow-up meeting, announced at that time to be held in August 2008, has yet to be scheduled.
By Cynthia E. Keen
AuntMinnie.com staff writer
June 23, 2009
Related Reading
Computer-aided system increases detection of early-stage lung cancer, May 4, 2009
Riverain scores regulatory approvals, November 19, 2008
Criteria determine CAD mark sensitivity, March 20, 2008
CAD provides mixed benefits for DR lung exams, March 8, 2008
CAD vendors hope FDA hearings will clear approval bottleneck, March 4, 2008
Copyright © 2009 AuntMinnie.com