Conventional Brain Scintigraphy:
Diseases of the brain cause a breakdown in the blood brain barrier which permits the uptake of conventional brain imaging agents. Other than for brain death, conventional brain scintigraphy is no longer routinely performed. Imaging agents included Tc99m-Pertechnetate, Tc99m-Glucoheptonate, or Tc99m-DTPA.
Tc99m-Pertechnetate in Conventional Brain Imaging:
Inexpensive and readily available, but has prolonged blood pool activity and is concentrated in the choroid plexus and salivary glands. This latter uptake can be prevented by ingestion of perchlorate.
Tc99m-DTPA in Conventional Brain Imaging:
Tc99m-DTPA has been preferred by some because of its more rapid blood clearance, and lack of salivary and choroid plexus activity.
Scintigraphic Findings in Conventional Brain Imaging:
Brain Death: (See also Tc-HMPAO
imaging)
Brain death is usually diagnosed by physical examination alone
[3]. Prerequsites to diagnosing brain death by physical exam
include a sufficient mechanism of injury, lack of confounding
factors (such as drug intoxication or poisoning), and exclusion of
complicating medical conditions that interfere with clinical
assessment (including facial trauma, pupillary abnormalities,
hypothermia, or severe electrolyte, acid-base, or endocrine
disturbances) [3].
Examination:
Dynamic images are obtained at 2 sec./ frame following a good bolus injection of the tracer (typically Tc-DTPA). Immediate anterior and lateral views of the skull are then performed. Delayed images are not required, in fact, superior sagittal sinus activity may be seen on delayed images due to a small amount of activity from the external circulation. A scalp tourniquet may be used to minimize scalp activity from the external carotid arteries, however, it is contraindicated in children since it may increase intracranial pressure.
Interpretation:
Absence of cerebral perfusion on planar imaging does not equate
with
brain death [2]. Specific clinical criteria for brain death are:
The
patient must have total absence of brain
stem reflexes, including no spontaneous respiration; and
potentially
reversible causes
must be excluded (such as drug intoxication (barbiturates),
hypothermia, or metabolic
derangement's). Additionally, the cause of the brain dysfunction
must
be diagnosed-
trauma, stoke, etc. The clinical findings of brain death must be
present for a defined
period of observation. For patients that meet the clinical
criteria for
brain death, a lack of blood flow to the brain is fairly
diagnostic of
brain death and is
usually the result of increased intracranial pressure. The
radionuclide
test is not
affected by drug intoxication or hypothermia as the EEG may be,
and is
more specific for
brain death. A lack of flow above the base of the skull on the
radionuclide angiogram in
conjunction with an absence of brain stem reflexes is strong
evidence
for brain death. Rare false negative exams may occur in patients
that
have open head injuries or craniotomies presumeably because of the
resultant decreases in intra-cranial pressure which allows flow
through
the intracranial areries [2]. Other rare reports of false negative
studies can be seen in patients with extensive liquifaction
necrosis of
the brain and in children with incompletely ossified skulls [2].
Scintigraphic findings compatible with brain death
- Lack of intracranial arterial flow: the carotid arteries are visualized in the neck, but there is an abrupt cut-off of activity at the skull base because increased intracranial pressure exceeds cerebral perfusion pressure [1].
- Sagittal/Venous sinuses are not visualized on subsequent static images
- The "hot nose" sign: The hot nose sign is due to decreased flow within the internal carotid arteries and increased flow in the external carotid circulation [1]. The hot nose sign can be seen in 52% of patients with brain death [1]. However, other authors indicate that the hot nose sign is neither specific or sensitive for brain death and is therefore unreliable [3]. The hot nose sign can be seen in association with other conditions that result in diminished blood flow in one or both internal carotid arteries including- CVA, subdural hematoma, or hepatic encephalopathy [1].
- Faint visualization of the venous sagital or transverse sinus in the absence of intracranial perfusion may be seen in 10-20% of patients. These patients almost invariably progress to death within days.
|
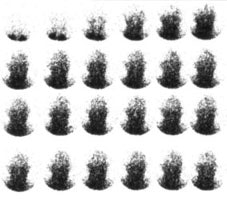
Brain death exam: The flow images demonstrated absent intracerebral flow, no sagittal sinus activity, and a hot nose sign- these findings are consistent with brain death.. |
|
|
|
Brain death exam- patient not dead: The flow images demonstrated intracerebral flow which was somewhat asymmetric. Later images revealed activity in the sagital sinus. A tourniquet had been placed around the skull to decrease scalp acitivity, but some scalp activity can still be seen. There is no "hot nose" sign. The exam indicated that the patient was not brain dead. |
|
|
Cerebral Vascular Accident:
Diminished activity in the involved vascular distribution during the arterial and capillary phases is characteristically seen during the first days after a stroke (subacute phase). Occasionally, increased perfusion may be seen with a recent stoke due to "luxury perfusion." This represents an uncoupling of blood flow from metabolism (excess perfusion relative to reduced oxygen consumption) and may be seen by about five days after the acute event. Sensitivity is best for carotid and middle cerebral artery infarctions and worse for anterior cerebral or vertebral-basilar artery infarcts.
The "Flip-Flop Phenomenon" is seen in CVA's due to delayed arrival of radiotracer at the site of an infarct via collateral vessels coupled with delayed washout from this area. This finding may also be seen with high grade carotid artery stenosis without infarction. The sign is characterized by:
- Decreased arterial perfusion
- Equalization of activity during the capillary phase
- Increased activity in the dynamic (venous) phase compared to
the
normal side.
Inflammation:
Blood flow is invariably increased to inflammatory lesions. Abscesses show increased activity on delayed images, and may have a "doughnut" appearance. Again, these findings are not specific and may be seen with neoplasms and rarely infarction. Herpes encephalitis will demonstrate increased flow and increased uptake on delayed images within the temporal lobe. Ventriculitis shows a pattern of bilateral increased lateral ventricle activity.
Trauma:
Dynamic flow images often show peripherally decreased activity due to mass effect. Delayed images reveal a peripheral increase in activity over the involved convexity ("crescent sign"). This finding is not specific and can also be seen with infarction or scalp trauma. Activity generally increases over time and delayed images are sometimes helpful. The study is most sensitive for subacute or chronic subdurals due to the presence of a well organized membrane (requires 10 or more days to form).
REFERENCES:
(1) Radiology 2005; Huang AH. The hot nose sign. 235: 216-217
(2) Radiographics 2013; Uliel L, et al. Nuclear medicine in the
acute
clinical setting: indications, imaging findings, and potential
pitfalls. 33: 375-396
(3) J Nucl Med 2016; Zuckier LS. Radionuclide evaluation of brain
death in the post-McMath era. 57: 1560-1568