CHICAGO - The widespread adoption of prostate cancer screening modalities such as the prostate specific antigen (PSA) test and transrectal ultrasound (TRUS) has led to an avalanche of prostate cancer diagnoses. In the U.S. nearly 189,000 men will be diagnosed with prostate cancer in 2002, and an estimated 11,200 will die from the disease, according to the American Cancer Association.
Interest in prostate cancer has led to a vigorous search for treatment modalities that are less invasive and debilitating than the gold standard, radical prostatectomy. Depending on disease severity, current treatment alternatives for locally confined prostate cancer range from watching and waiting to medical and surgical castration, and targeted radiotherapy.
Brachytherapy, while not recommended for locally advanced disease, comes with fewer side effects, including a lower rate of impotence (20-40%), compared to other treatment methods. Current investigational techniques include radiofrequency or microwave ablation, as well as cryoablation using liquid nitrogen or argon gas as a coolant.
At Tuesday's RSNA genitourinary sessions, Dr. Duke Bahn from the Crittenton Prostate Center in Ventura, CA, discussed a seven-year study of patients treated with cryoablation therapy. In years of careful follow-up, the group has found overall excellent results with its freezing technique.
"The objective of this study is to review the efficacy and safety of our long-term experience with targeted cryoablation of the prostate as a primary treatment for prostate cancer," Bahn said.
From March 1993 to September 2001, Bahn, Dr. Fred Lee Sr. and colleagues examined and treated 590 consecutive patients with prostate cancer. Color Doppler ultrasound was used for transrectal ultrasound (TRUS) examination and biopsy guidance. Ultrasound was also used to guide the cryogenic prostate ablation system developed by Endocare of Irvine, CA.
Based on TRUS examination, PSA and biopsy results, Bahn and colleagues divided patients into three groups:
Low risk: Stage ≤2A, PSA ≤10 mg/ml, Gleason grade ≤6
Medium risk: Stage ≥2B, PSA >10 mg/ml, Gleason Grade >7
High Risk: Two or more of the medium risk indicators
"Preoperative ablation therapy is (used) to cut down the size of the prostate," Bahn said. "Too large a prostate and we cannot freeze the entire prostate effectively. "
After creating a "cryromap" to plan the procedure, the radiologist ablates the entire prostate gland. Tissue necrosis results from the rupture of cell membranes due to ice crystal formation, Bahn said. With ultrasound guidance,2 to 8 cryogenic needles called cyroprobes (3.4 mm) are percutaneously inserted into the prostate in order to ablate the prostate tissue at temperatures of -68 to -70 C. The procedure takes less than 10 minutes.
"Preoperative identification of exact location and staging of the cancer utilizing color Doppler ultrasound is very important. That's where our role as radiologists kicks in," Bahn said.
During the procedure, temperature monitors are placed at various locations, a ureteral warming catheter is inserted, and care is taken not to freeze the sphincter, which is maintained at 11 degrees C or higher, he said.
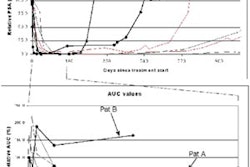
The patients remained at the facility overnight for observation, and then returned for biopsy at 6 months, one year, 2 years and five years. PSA is assessed every three months for a year, and every six months thereafter. All patients fill out questionnaire regarding complications after each visit; the mean follow-up for the study was 5.7 years, Bahn said.
The 7-year biopsy-proven disease-free rates were 87%, 92% and 77% for the low-, medium-, and high-risk groups, respectively. The biochemical disease-free rate was 87% for low-risk patients when PSA ≤1.0 mg/ml was used as an endpoint; and fell to 79% and 71% for medium and high-risk groups respectively, Bahn said.
As for complications, the most prevalent was impotence in 85% of patients. Incontinence was seen in 4.3% of the cohort, while 9% had a ureteral stricture. Rectal fistula was observed in 0.3% of the patients.
"Cryosurgery is an efficacious modality for organ-confined, and especially locally advanced T3-T4 (stage) prostate cancer," Bahn concluded. “(It) is a minimally invasive procedure, but unfortunately has a very steep learning curve."
By Eric Barnes
AuntMinnie.com
staff writer
December
4, 2002
Related Reading
Nerve-sparing
cryosurgery for prostate cancer can preserve potency, August 9, 2002
Brazilian
team finds success with cryosurgery for breast lesions, December 14, 2000
Copyright © 2002 AuntMinnie.com