Prostate-specific membrane antigen (PSMA) PET/CT imaging can reveal metastatic bone cancer lesions in prostate cancer patients that may be undetected by conventional bone scintigraphy, according to a group in the Netherlands.
In a first head-to-head comparison, researchers at Amsterdam University Medical Centers compared the performance of F-18 PSMA-PET/CT versus bone scintigraphy in high-risk prostate cancer patients. In 20% of patients, the results of PSMA-PET/CT imaging changed the intended treatment advice of specialists due to either upstaging or downstaging of disease, they found.
The findings could have major consequences for these patients, according to the authors.
"Those who are upstaged may undergo (palliative) systematic therapy more often instead of treatment with curative intent," wrote corresponding author Dr. Yves Bodar, in a study published December 30 in Urologic Oncology.
European guidelines currently recommend PSMA-PET/CT imaging for patients with biochemically recurrent prostate cancer after curative treatment. However, its value for staging of primary prostate cancer is yet unknown, especially since major studies based on patients with primary metastatic prostate cancer still rely on conventional imaging, according to the researchers.
"This is the first prospective, multicenter, head-to-head comparative study that assessed the bone lesion detection rates of conventional [bone scintigraphy] and F-18 PSMA-PET/CT for primary staging of prostate cancer," they wrote.
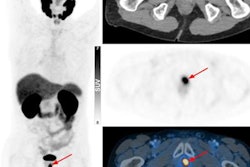
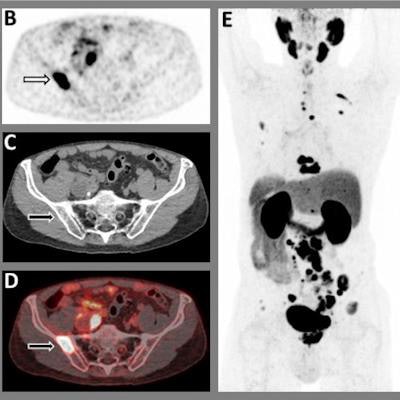
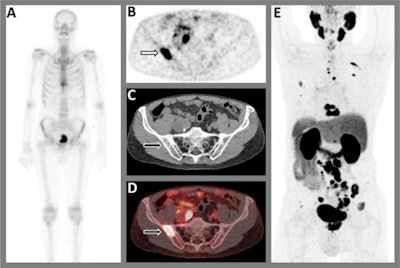 A 75-year-old patient with biopsy-proven prostate cancer. (A) Tc-99m bone scintigraphy axial images show increased bone activity in two thoracic vertebrae (Th9 and Th10) that were classified as (osteoporotic) compression fractures, and the faint uptake in the left third rib was attributed to a post-traumatic origin. Although there was a clear high-risk profile in this patient, there was no suspicion for bone metastases. (B) transversal reconstruction of F-18 PSMA-PET at pelvic region, (C) CT and (D) fused PET/CT images show a suspicion for a bone metastasis in the right iliac bone, in contrast to the bone scintigraphy. Moreover, an extensive suspicion for lymphogenous and osseous metastatic lesions were found throughout the body, as shown on (E) PET axial images. Based on the F-18 PSMA-PET/CT results, the patient was treated with androgen deprivation therapy in combination with abiraterone. Image and caption courtesy of Urologic Oncology and licensed under CC BY 4.0
A 75-year-old patient with biopsy-proven prostate cancer. (A) Tc-99m bone scintigraphy axial images show increased bone activity in two thoracic vertebrae (Th9 and Th10) that were classified as (osteoporotic) compression fractures, and the faint uptake in the left third rib was attributed to a post-traumatic origin. Although there was a clear high-risk profile in this patient, there was no suspicion for bone metastases. (B) transversal reconstruction of F-18 PSMA-PET at pelvic region, (C) CT and (D) fused PET/CT images show a suspicion for a bone metastasis in the right iliac bone, in contrast to the bone scintigraphy. Moreover, an extensive suspicion for lymphogenous and osseous metastatic lesions were found throughout the body, as shown on (E) PET axial images. Based on the F-18 PSMA-PET/CT results, the patient was treated with androgen deprivation therapy in combination with abiraterone. Image and caption courtesy of Urologic Oncology and licensed under CC BY 4.0The researchers enrolled 79 patients with high-risk prostate cancer between March 2019 and July 2021 at two local hospitals. The patients were prospectively staged using bone scintigraphy and subsequent F-18 PSMA-PET/CT before initial therapy.
Out of 70 patients with a bone scintigraphy scan negative for metastases on primary staging, at least one bone metastasis was visualized on subsequent F-18 PSMA-PET/CT in 12.9% (9/70) of patients. In patients with low-volume metastatic disease on bone scintigraphy, upstaging to high-volume metastatic disease was reported in four of nine patients (44.4%), and downstaging to absence of bone metastatic disease in two of nine patients (22.2%), according to the findings.
"We found that in almost 20% of patients, the results of F-18 PSMA-PET/CT imaging changed the intended treatment advice due to either upstaging or downstaging of disease," the authors wrote.
One limit of the study was that different F-18 PSMA-PET radiotracers were used and that different scanning protocols were used within the two hospitals, which might have influenced the interpretation of the study results, the authors noted.
Nonetheless, the results are promising and warrant further research into whether PSMA-PET can add value in primary staging of these patients, the authors suggest.
"Further studies are needed to assess what the exact consequences are of modern staging on more mature oncological outcomes, such as time to metastatic castration-resistant disease or overall survival," Bodar and colleagues concluded.