SAN FRANCISCO – While research forges ahead on the use of MRI as a tool for breast cancer staging and screening, clinicians need to keep in mind that this highly sensitive modality can sometimes give patients too much information -- information that they may, in retrospect, decide they don't want.
In a presentation April 9 at the American College of Radiology's National Conference on Breast Cancer in San Francisco, Dr. Susan Greenstein Orel cautioned attendees that one of the limiting factors of using MRI for breast cancer staging is its ability to pinpoint problems that either may not require treatment or for which treatment is still undetermined.
"Are we finding and acting on disease when we didn’t have to? It’s important to discuss the MRI with the patient and make sure they understand what the benefits and drawbacks of this exam are. A woman with lesions in one breast may not want to have the contralateral breast examined," said Orel, associate professor of radiology at the Hospital of the University of Pennsylvania in Philadelphia. "In some cases, patients don’t want to know."
One gray area in breast MRI that can cause confusion is the clinical significance of breast cancer detected with MRI. For example, would radiation therapy or excision be the best way to treat lesions detected with MRI? If multiple lesions are identified by MRI, how many, if any, should be localized?, Orel asked.
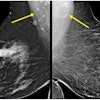
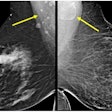
Another limiting factor of MRI for imaging breast lesions is that both benign and malignant lesions can demonstrate contrast enhancement, not only in cancerous lesions, but also in fibroadenomas, fat necrosis, and radial scars. In addition, normal breast tissue may enhance following contrast agent administration, and these results can vary with different phases of the menstrual cycle. Reported specificity ratings of breast MRI vary, from 37% to 97%, Orel said.
Still, with reported sensitivity rates for breast cancer detection and diagnosis closing in on 100%, MRI has the potential to be a reliable adjuvant modality, picking up where mammography leaves off. MRI has shown great promise as a staging method for newly diagnosed breast cancer prior to excisional biopsy. The modality also can identify the extent of residual disease following excisional biopsy at the margins or resection. Finally, MRI has been able to find axillary node malignancy when mammography failed to do so, Orel said.
Orel stated that breast MRI is still in the investigational stage, and outlined some of the areas that require further evaluation:
- A standard technique for MRI of the breast needs to be created. General technical issues that need to be addressed include the suppression of fat signal (enhancing lesions may not be detected, as they become isointense to fat following contrast administration). The trade-off between temporal resolution and spatial resolution also requires additional discussion.
- An MRI-guided biopsy system is needed to obtain histologic diagnosis of lesions. A major limitation of MRI-guided needle localization is its inability to verify lesion removal because MR-identified lesions are not visible with mammography.
- The price tag associated with MRI breast screening is still prohibitive. At Orel's institution, MRI exams are billed at about $2,000 per hour, she said. "There’s no doubt whether MR will find (cancers), but whether it’s cost-effective, we don’t know," she added.
In conclusion, Orel referred NCBC attendees to current breast MRI research published in the April 2000 issue of Radiology, in which German researchers reported on a prospective trial comparing MRI to conventional imaging for screening high-risk women.
Conducted at the University of Bonn Medical Center, researchers imaged 192 asymptomatic women and six symptomatic women who either had a family history of breast cancer or were suspected carriers of a breast cancer susceptibility gene. Out of that group, 15 breast cancers were identified: nine in the 192 asymptomatic women and six in the symptomatic. In 105 asymptomatic women, mammography and ultrasound had sensitivities of 33%, while MR had a sensitivity of 100%. MR imaging allowed the correct classification and local staging of all nine cancers, the group reported.
By Shalmali Pal
AuntMinnie.com staff writer
April 11, 2000
Let AuntMinnie.com know what you think about this story.
Copyright © 2000 AuntMinnie.com