Automated breast volume scanning (ABVS) shows promise in predicting pathologic response in women with breast cancer, suggest findings published January 13 in Clinical Radiology.
A team led by Dr. Yuan Peng from Peking University People's Hospital in China reported that ABVS had higher accuracy rates than mammography, ultrasound, and MRI when it came to estimating tumor size.
"For predicting complete pathologic response ... ABVS is significantly better than mammography, and the area under the receiver operating curve [AUC] is higher than ultrasound and MRI, [although] without statistical advantages," Peng and colleagues wrote.
While multiple imaging methods can assess breast tumor size after neoadjuvant therapy, no standard method currently exists to assess pathologic response, with each method having its respective pros and cons.
While ultrasound is frequently used, its performance varies depending on operator skill and it has typically demonstrated poor repeatability. Mammography's performance suffers when imaging dense breast tissue, and MRI has shown it can both under- and overestimate residual disease (and MRI is expensive and cannot be used on patients who are allergic to contrast agents or have metal implants). However, ABVS is a new technique that covers the whole breast using an automated ultrasound system at frequencies of 5 to 15 MHz.
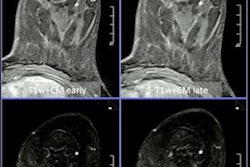
Peng and colleagues investigated the performance of ABVS for assessing residual breast tumor size after neoadjuvant therapy, comparing it to hand-held ultrasonography, mammography, and MRI.
The group included data collected between 2016 and 2020 from 156 women with a total of 159 breast tumors in their study. Of the tumors included in the study, 57 showed complete pathologic response.
The researchers found that ABVS had higher intraclass correlation coefficient (ICC) values and coincidence rates than the other imaging modalities, with a 5 mm tumor size threshold.
| Comparison between mammography, ultrasound, MRI, and ABVS for accurately predicting residual breast cancer after neoadjuvant treatment | ||||
| Measure | Mammography | Ultrasound | MRI | ABVS |
| ICC values (with 1 as reference) | 0.432 | 0.546 | 0.595 | 0.666 |
| Accuracy rates | 45.8% | 52.5% | 43.9% | 65.4% |
| AUC | 0.788 | 0.816 | 0.819 | 0.855 |
The researchers also found that among different subtypes, although MRI showed high agreement in triple-negative breast cancer (ICC value, 0.733), ABVS showed higher agreement, with an ICC value of 0.797.
ABVS also showed the largest AUC values among all modalities in HR+/HER2- tumors (0.929), HR+/HER2+ tumors (0.933), and HR-/HER2+ tumors (0.825) and had the highest positive predictive value in HR+/HER2- and HR+/HER2+ tumors.
Based on the study results, ABVS could be effective in evaluating post-treatment lesions, the investigators reported. They also noted that the advantages of ABVS include its repeatability, its efficiency compared with conventional ultrasound, and the fact that it doesn't require contrast agents.
Despite these benefits, Peng and colleagues noted that ABVS has the same shortcomings as conventional ultrasound, including difficulty in distinguishing residual tumors from post-treatment fibrosis and shadow artifacts caused by the nipple. But even with these limitations the technique shows good agreement with pathology after treatment in suitable patients.
"These findings remind us that ABVS could be a potential tool for assessing tumor response to neoadjuvant therapy, especially for patients with contraindications to MRI or to avoid operator dependence bias of ultrasound," they wrote.