The growing challenge of viewing and managing the growing mountains of image data generated in radiology today has drawn considerable attention, and there was no better place to learn about this topic than the 20th Symposium for Computer Applications in Radiology in Boston.
The Society for Computer Applications in Radiology (SCAR)’s Transforming the Radiological Interpretation Process (TRIP) initiative was the focus of the closing session at this year’s show. TRIP is designed to spearhead research, education, and discovery of approaches to the problems of information and image data overload, according to the Great Falls, VA-based society.
This topic was also the subject of a SCAR University talk presented by Dr. Eliot Siegel, professor and vice chairman of information systems at the University of Maryland School of Medicine in Baltimore. In his presentation, Siegel made the case for a volumetric approach to image navigation.
With volumetric navigation and multiplanar and 3-D imaging, the process of image review can be separated from the manner in which they were acquired and reconstructed, Siegel said. For example, CT scanners for the most part acquire images in the axial plane, but with isotropic, thin-section imaging, the radiologist is free to navigate the patient data volume in an unlimited number of ways.
The growing power and utility of flat-panel displays was evident in several presentations at the meeting. In one talk, researchers from Massachusetts General Hospital presented preliminary research comparing consumer-grade color flat-panel monitors with medical-grade, high-luminance monochrome cathode-ray tube monitors for the primary diagnosis of abdominopelvic CT exams.
A five-megapixel medical-grade monochrome liquid-crystal display (LCD) with up to 200 foot-lamberts of brightness can range in price from $15,000 to $20,000, while a consumer-grade two-megapixel color display rated at 80 foot-lamberts can cost approximately $750 to $1,000. Although not suitable for the high-brightness and resolution demands required for radiographic studies, the lower-end display can more than handle the 0.25-megapixel resolution of CT studies, according to MGH’s Dr. David Hirschorn.
As part of research to test their hypothesis that there's no significant difference between consumer-grade flat-panel displays and the monochrome medical-grade CRT displays, the MGH research group queried seven of its radiologists for subjective comparisons of the two systems.
Four out of the seven radiologists were as confident with their diagnosis in general with the flat-panel display as they were with CRTs, with one slightly less confident and two who didn't know. Five of the radiologists had the same level of confidence in looking at calcifications, one had slightly less, and one didn't know. For conspicuity of hemorrhage, four said they were as confident, one slightly less, and two said they didn't know.
One radiologist was more confident with tumor conspicuity with the flat-panel display, four had the same level of confidence, one had less confidence, and one didn't know. For edema in fat, three were as confident, one was less confident, two were slightly less confident, and one didn't know.
All seven said they preferred having PACS and speech recognition on a single computer with one mouse and keyboard. As for general preference between the flat-panel and CRT systems, it was a wash, Hirschorn said.
Training makes the difference
In PACS, a solid training program can make all the difference. At Texas Children’s Hospital in Houston, a mandatory training program that utilized basic PACS training modules was a critical factor in the success and acceptance of the institution’s digital image management system.
During a five-year project to convert to a filmless environment, TCH noticed that issues often came up between administrators, analysts, and users, said Maria Elissa Elevado Blado.
To address the problem, TCH developed and documented PACS-related tasks and also generated a list of PACS terms applicable to the department. All of these items were consolidated into PACS training modules, which were eventually incorporated into a PACS training manual. The modules included:
- Definition of PACS terms.
- A list of equipment and networks.
- Function of equipment and networks.
- Quality control of equipment.
- Service/problem solving.
- Flow, retrieval, and archive of images.
- Protocols.
- Downtime procedures.
- Communication.
The modules, which were eventually incorporated into a PACS training manual, were presented as part of a mandatory two-hour training session. The training program has been a big success, leading to less user intimidation with the PACS network. And even long-time PACS users gained additional knowledge, she said.
Getting rid of paper
Among other presentations, researchers from Maine Medical Center in Portland, ME, concluded that eliminating the use of paper can confer additional efficiencies on a radiology department’s workflow. MMC created lists of the type of paper forms generated in a pre-PACS environment, and identified which forms could be replaced
Converting to a paperless approach proved beneficial for the film library, radiologists, the transcription department, technologists, and the referring clinicians alike, said MMC radiologist Dr. Mathew Ralston.
Paperwork for the film library was almost completely eliminated, according to Ralston. As a PACS, by definition, means that there are no more film jackets, this paper form was abolished. For the radiologists, the group has managed to create a system whereby any exam performed in the system can be interpreted from any workstation without the need for a paper requisition form or a printed schedule.
The team also created an application interface that replaced the paper-based peer-review process used in the institution’s pre-PACS era. The new process uses PACS keywords and comments fields and is preferred over the previous procedure, noted Ralston.
The facility uses transcriptionists instead of a voice-recognition system, and has trimmed report turnaround time to two hours, primarily due to the abandonment of a hard-copy transcription request form. This form, Ralston said, was frequently prone to snags, such as being lost or misplaced.
The PACS network has been integrated with a digital dictation system that automatically routes an order number to the transcription department on completion of a radiologist’s read. This ensures that the voice file is immediately available to the transcriptionists and can be worked on without waiting for paperwork.
Ralston advised that institutions that are adopting PACS specify and build their system to allow for a paperless transition. He also cautioned the SCAR audience that they should focus on one subset of paperwork to eliminate at a time. This ensures that the transition to electronic orders is systematic and not a chaotic mix of paper forms combined with electronic transactions.
Docs like it online
In a notable poster presentation, Dr. Biswata Mozumdar from the National Institutes of Health in Bethesda, MD, reported that referring physicians prefer online scheduling of radiology procedures compared with the traditional telephone method.
The NIH researchers conducted an email survey of 60 physicians who referred patients to a single, large academic radiology department. Of the 33 survey respondents, 26 (78.8%) indicated they were willing to try to schedule online. Sixteen of the 26 actually tested the system.
Two staff members were interested in online scheduling, but did not have online access. The researchers gathered from interview results that the others did not have the option to schedule online.
Of the 16 respondents who tried online scheduling, 12 said it was an easier method of scheduling patients. Three (18.75%) said the online system did not simplify scheduling, citing difficulties with patient preparation and arrival time. One user did not indicate a preference, according to the researchers.
Eleven of the 33 survey respondents told the researchers that they changed providers if they were dissatisfied with the patient scheduling experience at a particular provider. Of the 16 who tried online scheduling, five (31.25%) said their choice of radiology service providers would be subject to change due to scheduling ease, the authors wrote.
Online scheduling applications are becoming the preferred scheduling vehicle, the authors concluded. Augmenting their capabilities and availability can simplify the scheduling process, increase efficiency, improve referring physician satisfaction, and provide a competitive advantage. Referrers are willing to change providers if scheduling expectations are not met, they noted.
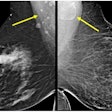
Size matters with FFDM detectors
Those contemplating employing a full-field digital mammography (FFDM) system for mobile screening might take note of research from the University of Texas M. D. Anderson Cancer Center (MDACC) in Houston. The MDACC researchers concluded that a 21 x 29-cm image receptor may be the optimal choice for high-volume digital screening applications.
To determine whether a 19 x 28-cm detector would be feasible for high-volume, mobile digital mammography screening applications, the researchers obtained mobile film-screen mammograms on 322 consecutive women at 15 sites using either a 18 x 24-cm receptor or a 24 x 30-cm receptor. Four measurements were performed, and the data was extrapolated to determine the optimal size for an FFDM detector.
The researchers concluded that 305 cases (95%) could be imaged with a 19 x 27-cm digital receptor. However, a 21 x 29-cm detector with a 2-cm anterior margin and a 1-cm margin at each end would also be practical for that same 95%, while providing a margin of about 1 cm on each end and probably a centimeter or two anteriorly, said Dr. Gary Whitman.
This provides a margin of positioning error for technologists and allows easier evaluation of skin and superficial tissues, he said.
Attendance at this year’s meeting exceeded 2,600, an increase of over 25% over the 2002 show. In 2004, SCAR moves north of the border to Vancouver, where the meeting will be held May 20-23 at the Vancouver Convention and Exhibition Centre.
By Erik L. Ridley
AuntMinnie.com staff writer
October 7, 2003
Copyright © 2003 AuntMinnie.com