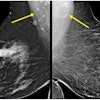
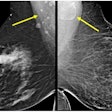
As expected, radiologists who specialize in mammography have a better track record for detecting cancers than those who read mammograms as part of their general practice. But the addition of a multiple-reading system can improve the latter group’s results.
In a study published in the September issue of Radiology, Drs. Edward Sickles and Dulcy Wolverton from the University of California, San Francisco, along with Dr. Katherine Dee from the University of Washington Medical Center in Seattle, evaluated the performance parameters for breast imaging specialists and general diagnostic radiologists who interpreted a large series of consecutive and diagnostic mammographic studies.
For the study, data was collected from all screening and diagnostic mammograms performed at either the Breast Imaging Center (BIC) or the Ambulatory Care Center (ACC) in San Francisco. At the BIC, at least two residents and one breast imaging fellow reviewed all exams before a staff radiologist rendered a final interpretation. A radiologic-pathologic correlation conference was then held. Three breast imaging specialists, who interpreted more than 5,000 mammograms per year, read at the BIC, as did some general radiologists.
At the ACC, three general diagnostic radiologists, all of whom met the minimum standard of reading 960 examinations per 2-year period, interpreted the mammograms. However, at the ACC a single rather than multiple-reading protocol was used, as there were no residents or fellows on duty. Correlation with pathology was limited to personal review by the staff radiologist.
"For both screening and diagnostic mammographic examinations, we calculated abnormal interpretation rates by dividing the number of abnormal interpretation rates by the number of studies interpreted," the authors explained. Biopsy rates were calculated by dividing the number of abnormal examinations for which biopsy was performed by the number of studies interpreted; the same formula was used for determining cancer diagnosis (Radiology, September 2002, Vol.224:3, pp. 861-869).
The study involved 47,798 screening exams. Previous mammograms were available for 54.6% of the exams read by specialists and 54.3% of the studies read by general radiologists. In this patient population, the abnormal interpretation, or recall, rate was 4.9% for the specialists and 7.1% for the general radiologists. The biopsy rate was 1.5% for the breast imagers, and 1.1% for the general readers. The cancer detection rate was 6 cancer cases per 1,000 exams for the mammographers and 3.4 cancer cases per 1,000 exams for the general radiologists.
Out of the total of 61,083 exams, 13,286 were classified as diagnostic. Previous mammograms were available for 66.6% of the exams read by specialists and 66.1% read by non-specialists. In this group, the recall rate was 15.8% for breast imagers and 9.9% for general rads. The biopsy rate was 12.3% for mammographers and 7.5% for general readers. Finally, the cancer detection rate was 59 cancer cases per 1,000 exams for the specialists and 36.6 cancer cases per 1,000 exams for the general radiologists.
"The detection rates for less advanced (stage 0 or I) cancers were higher among specialist radiologists than general radiologists," the authors stated. "The most striking differences in (performance) were observed between our three specialist radiologists and the seven general radiologists, who interpret mammograms less frequently…the specialist radiologists make more true-positive and fewer false-positive interpretations at screening mammography. At diagnostic mammography, the specialist radiologists make more true-positive and more false-positive interpretations."
The group attributed the latter to a higher, and preferable, level of performance, as "the principal goal of mammography is cancer detection rather than reduction of benign biopsy results."
Finally, general radiologists at the BIC fared better than general radiologists at the ACC because of the multiple-read protocol used at the BIC, the paper stated.
"This multiple-read system is similar to the second-look type of double reading that is performed by computer-assisted detection (CAD) software programs," the authors wrote. "We conclude that the observed differences in performance between BIC and ACC general radiologists in our practice are a result of multiple- versus single-reading interpretation."
By Shalmali PalAuntMinnie.com staff writer
September 6, 2002
Related Reading
Reading mammograms: the good, the bad, and the suspicious, July 3, 2002
CAD algorithm spots spiculated malignant masses in breast, July 2, 2002
CAD technology begins to make good on its promise, March 14, 2002
Mammography reader volume directly linked to diagnostic accuracy, March 6, 2002
CAD cuts false negatives, increases sensitivity of breast imaging, November 28, 2001
Copyright © 2002 AuntMinnie.com