Breast biopsy has evolved dramatically over the past 20 years -- and for good reason. Just 25% of the 1.2 million breast biopsies performed each year prove positive for cancer, leading providers, patients, and payors alike to push for more effective and less invasive ways to determine breast lesion malignancy.
The heavy reliance on open surgical procedures in the 1980s gave way to growing acceptance of percutaneous core-needle biopsy in the 1990s. Along the way, flirtations with fine-needle aspiration biopsy (FNAB), initially promising as a minimally invasive technique, fizzled due to a high insufficiency rate for nonpalpable masses.
Aided by the introduction of automated biopsy guns in the early 1990s, more than 80% of radiologists by 1997 were performing core-needle biopsies of suspicious masses and calcifications. The core technique has many advantages compared to surgery, including:
- Use of local anesthesia
- Shorter procedure and recovery time
- Minimal patient discomfort
- No permanent scarring
Clinical experience with the technique led the Health Care Financing Administration (now the Centers for Medicare and Medicaid Services, CMS) in 1999 to declare minimally invasive, image-guided core-needle biopsy as accurate as open surgical biopsy in the breast.
The introduction of the first vacuum-assisted biopsy (VAB) device in 1996 sparked debate over which of the two techniques is best. Imaging techniques have also evolved for biopsy guidance, from standard stereotaxis to ultrasound. And the potential to achieve total lesion excision has prompted the introduction of devices capable of obtaining even larger core samples while spurring controversy over how much tissue is too much.
Clinical applications
Core-needle biopsy. A wealth of evidence exists supporting the clinical value of core-needle biopsy as compared to open surgical biopsy; less literature is available comparing the automated gun technique with vacuum-assisted devices. Both techniques require only a small (1/4 to 3/4-inch) incision, and either can be performed under stereotactic or ultrasound guidance.
Generally, a biopsy is indicated when screening-detected lesions fall into BI-RADS categories 3, 4, or 5, including clustered microcalcifications, spiculated masses, focal densities, or solid masses.
The automated biopsy gun relies on a spring-loaded, two-step firing device that uses a notched needle to advance through the lesion, followed by a cutting cannula that cuts the tissue specimen and collects it in a notch. The needle is removed from the breast to retrieve the sample.
Key advantages of core-needle biopsy include ease of use; low-cost (biopsy guns cost $1,500 on average, with disposable needles costing $50 each); and the ability to fire the needle into both dense breast tissue and firm lesions that can be otherwise difficult to penetrate. Downsides include the need to reinsert the needle with each pass, and a smaller specimen size than that obtained with VAB, raising the possibility of insufficient sampling, sampling error, or possibility of rebiopsy.
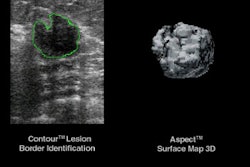
Vacuum-assisted biopsy. VAB devices use a dual-lumen needle or probe that is inserted into the breast once to obtain multiple tissue samples. The probe is advanced into the lesion and suction is applied through a narrow vacuum. A rotating cutter cuts and transports the tissue core outside of the breast to the collection chamber. After each sample is acquired, the probe is rotated clockwise to sample a new area of the lesion. The probe remains in the lesion during the entire procedure.
The advantages of VAB include a single probe insertion; larger samples, and thus less potential for sampling error; and the ability to obtain multiple samples in a short amount of time. In many instances, VAB can remove most or all lesions 1.5 cm or less in size. Disadvantages include cumbersome tubing, cost (which can average $10,000 for the device as well as $250 and up for disposable needle and components); and the potential for complications such as bleeding.
VAB devices in use include Mammotome, distributed by Ethicon Endo-Surgery of Cincinnati (available since 1996); MIBB from U.S. Surgical of Norwalk, CT, (1997), and ATEC from Suros Surgical Systems of Indianapolis (March 2002). The most extensive experience on record has been with the Mammotome.
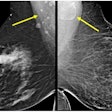
While VAB is being used to biopsy the full range of abnormalities seen on mammography and ultrasound, it appears most valuable in calcifications as compared to the core-needle automated technique. Patients with calcifications are most likely to benefit from VAB, particularly when stereotactic guidance and an 11-gauge needle is used, according to Dr. Laura Liberman, attending radiologist at Memorial Sloan-Kettering Cancer Center in New York City.
Similarly, in a study presented at the 2002 American Roentgen Ray Society meeting, Dr. Liane Philpotts also found that calcifications are better biopsied using VAB under stereotactic guidance. But she found no statistical difference between core needle and VAB in terms of false-negative findings in women with abnormal masses. Philpotts is an assistant professor of radiology at Yale University in New Haven, CT.
But Philpotts told AuntMinnie.com that hospitals should probably have both devices on hand, using the automated technique for sampling masses using ultrasound, while reserving use of VAB for calcified lesions because of its higher cost. "For masses, the VAB is not really necessary. But it is superior for calcifications," she said.
Not all agree. Based on a team study from eight facilities across the U.S. and Canada, Dr. Steven Parker, head of breast imaging at the Sally Jobe Breast Centre in Greenwood, CO, now recommends that all breast masses 1.5 cm and smaller be biopsied using VAB and ultrasound guidance.
Regarding technique, the optimal number of tissue samples typically required varies based on the appearance of the lesion. Fewer passes are needed for solid-appearing masses than for calcifications. At the 2001 RSNA meeting, Dr. Kimberly Wiele, an assistant professor of radiology at Washington University School of Medicine in St. Louis, reported 99.9% accuracy of ultrasound-guided core biopsy of masses in as few as three passes. Other researchers have shown that up to five passes may be needed when sampling calcifications with either the automated gun or the VAB.
The VAB technique may be easier for new recruits to learn. Achieving an acceptable success rate with stereotactic biopsy requires an average of 20 cases using a 14-gauge automated gun and an average of 15 cases for 11-gauge VAB, according to Liberman.
Image guidance
Ultrasound-guided core biopsy is being increasingly used due to its many advantages over the stereotactic technique, including speed, real-time visualization of the needle, and patient comfort.
At Yale, the majority of masses are biopsied under ultrasound guidance for convenience as well as patient comfort.
But ultrasound-guided biopsies using VAB may be more difficult in dense breasts. Firm lesions, and lesions located near the chest wall, may be easier to biopsy with the automated gun when ultrasound guidance is used. Without the compression used in stereotactic biopsy, the VAB probe may push away firm lesions such as fibroadenomas, Philpotts said.
Therapeutic potential
VAB devices go a step beyond standard core biopsy in their ability to remove a lesion in its entirety. While no vendor has yet approached the FDA for clearance of a VAB product as a therapeutic device, VAB is being increasingly tested as an excisional tool.
At the 2001 RSNA meeting, several researchers reported results from studies evaluating VAB’s performance in lesion excision. Dr. Annette Blank, an attending physician at Sourasky Medical Center in Tel Aviv, Israel, found that fibroadenomas can be completely eradicated with an ultrasound-guided VAB. All 20 fibroadenomas that were less than 1.5 cm in diameter were removed. Less successful was removal of larger lesions: of 11 fibroadenomas that were 1.5 to 2 cm, eight were totally removed. None of three lesions larger than 2 cm could be completely removed with the device.
Excision does not spell therapy, however, and experts do not agree that removing large tissue cores are necessary. The advantage of excising small lesions lies in reducing the possibility of false negatives and in providing a more accurate estimate of disease. Few radiologists today are performing biopsies with the goal of eliminating lesions, however.
"Even when you have real-time visualization with ultrasound, you can’t see histologically what you are doing, and often these excised lesions still have positive margins," Philpotts said.
Features and benefits
The Mammotome device has the longest -- and most published -- track record of any of the VAB devices. Less is known about U.S. Surgical’s MIBB device. The newest entry, the ATEC (Advanced Tissue Excision and Collection) system, was cleared by the FDA in March and is being used in 15 states. All of the above devices share the same benefits of VAB noted above, and each offers a handheld version.
Suros Medical Systems has positioned its ATEC device as the fastest biopsy tool on the market, able to obtain 16 cores per minute. The completely disposable device can be discarded after each procedure, unlike Mammotome, which requires cleaning of the driver after each biopsy.
The excision of entire lesions can eradicate landmarks and make post-biopsy follow up problematic. Clips and markers designed for placement in the biopsy cavity are available from multiple vendors, although their use is not foolproof. Clip migration after placement has been reported by some users, particularly after stereotactic biopsy. Once compression is released, markers that appeared accurately in place may have moved. Markers range from steel clips to a newly introduced collagen marker, and can be visualized on ultrasound and mammography.
Ethicon Endo-Surgery markets the steel Micromark marker, which is compatible with Mammotome; a similar product is the UltraClip from InRad of Kentwood, MI. Seno-Rx of Aliso Viejo, CA, is in beta testing with its second-generation gelatin marker, Gel Mark Ultra. Artemis Medical of Dartford, U.K., has developed the collagen-based self-expanding MammoMark, which resorbs within weeks, leaving behind a titanium clip for long-term follow up.
In addition to clips, several tools to assist in lesion targeting and visualization are available, but are relatively untried.
Click here for a list of breast biopsy device vendors.
Reimbursement
Medicare allows payment for minimally invasive, image-guided biopsies of nonpalpable lesions using CPT code 19102 (needle-core, automated-gun method) or code 19103 (vacuum-assisted or excisional biopsy device).
The new code for VAB was added in 2001, after extensive lobbying by vendors and physician specialty societies to the AMA to create a new code. The image-guidance component is coded 76095 (stereotactic-guided breast biopsy) or 76942 (ultrasound-guided needle biopsy).
In April, the Centers for Medicare and Medicaid Services issued a national coverage determination allowing for payment of image-guided biopsy of palpable lesions as well. A CPT code has not yet been assigned. The coverage is expected to become effective by fall 2002. A new code was also added in 2001 for placement of localization clips (CPT 19295).
Competitive devices
A trio of devices compete with VAB in the minimally invasive biopsy market. These large-core sampling systems are more excisional than incisional, and are categorized by some industry analysts as automated surgical devices. Target users include surgeons as well as radiologists.
The Advanced Breast Biopsy Instrumentation (ABBI) device from U.S. Surgical was introduced in 1997. The device removes a large, 2-cm core of tissue for sampling. The device requires stereotactic guidance for insertion of a large-bore (5-20 mm) cutting cannula that excises a lesion by removing a long cylinder of tissue.
Published research to date on ABBI has not been promising, although the device is in use in some centers. Three studies published in 1999 and 2000 detail problems with ABBI procedures, namely, a high percentage of positive margins for malignant lesions and poor performance as an excision tool. Other users have concluded that the procedure is needlessly more invasive than core biopsy and offers no advantage over the standard needle-core technique. One study noted a high number of complications and technical failures (American Journal of Roentgenology, July 1999, Vol.173:1, pp. 221-226).
The SiteSelect device from Imagyn Medical Systems of Irvine, CA, is also a large-core device but spares the tissue between skin and lesion, targeting only the 2-cm sampling area for excision. SiteSelect also requires stereotactic guidance. Imagyn has positioned the product as an alternative to VAB, ABBI, and open surgery.
According to the company, SiteSelect is superior to VAB because it removes a single tissue core instead of multiple samples; offers more definitive diagnosis of ductal carcinoma in situ (DCIS) and atypical ductal hyperplasia (ADH); and has less chance for rebiopsy, with no motors or vacuum required. When compared to ABBI, SiteSelect is simpler to use, carries the potential for less bleeding, and uses no motors or cautery, in addition to sparing tissue between skin and lesion, according to Imagyn.
Centrica from Sanarus Medical of Pleasanton, CA, is the only large-core biopsy device designed for lesion excision under ultrasound guidance. Newly cleared by FDA in March, Centrica consists of a console, a handheld device that houses the securing needle and cutting cannula, a sample tray, foot pedal, and regulator.
Centrica uses inert argon gas as a cooling agent that "stick freezes" the lesion after needle insertion. The tissue surrounding the needle is frozen and held in place. Once the lesion is stabilized, the cutting cannula rotates and advances over the needle and cores the specimen. The needle is retracted and the core delivered to the specimen container. The device has been commercially available since November 2001.
Philpotts of Yale questioned the necessity of large core samples, arguing that accurate diagnoses are already being made with existing techniques.
"Because of the difficulty of getting clean margins, it’s possible to remove this large core of tissue and still not get the entire lesion," she said. "Instead, you can make a diagnosis with a core biopsy needle and let the lesions that are positive be dealt with surgically."
Return on investment
There is little argument that core biopsy, at an average cost per procedure of $1,500, is more cost-effective than open surgical biopsy, which can cost up to $5,000. Generally, cost savings are higher with the automated gun procedure than with VAB, however. The cost of a stereotactic VAB is about 1.34 times that of the automated gun method. Cost savings are highest when ultrasound guidance is used, with either the automated or VAB approach.
Other factors need to be considered in the cost equation, however, according to Liberman of Memorial Sloan-Kettering. For example, in women with calcifications, use of VAB is significantly more likely to spare a surgical procedure, as well as yield a savings of $315 per case compared with surgical biopsy.
In a separate study that included 200 consecutive nonpalpable lesions, Liberman found that stereotactic, 11-gauge VAB decreased the cost of diagnosis by 20%, or $264 per case, when compared to surgical biopsy. Of the 200 lesions, 53% would not have been amenable to 14-gauge automated core biopsy because of their small size, superficial location, or inadequate breast thickness, she said.
Although the savings are modest, VAB expands the spectrum of lesions amenable to stereotactic biopsy, increasing cost savings, she said.
Another study comparing the cost advantages of VAB versus open surgical biopsy found that savings vary significantly depending on where biopsies are performed. In a study conducted at Kaiser Permanente in Sacramento, CA, researchers found cost savings for VAB of $314 to $843 per procedure, depending on facility type.
According to Dr. Balazs Bodai, chief of surgery at Kaiser Permanente and lead investigator in the study, the highest cost savings were seen when a VAB procedure was performed in an imaging center as compared to either a hospital or surgical center. In that environment, the cost of VAB was 62% less than open surgical biopsy.
"The total labor and supply cost difference between VAB and open surgical biopsy may be small, but the consideration of other cost savings such as those to patients, payors, and society may support adoption of VAB devices," Bodai noted in the May 2001 edition of the American Journal of Managed Care (May 2001, Vol.7:5, pp. 527-538).
Future
The future use of VAB and core-needle biopsy techniques will be guided by the application of new imaging modalities to breast imaging.
The use of contrast-enhanced MRI has shown value in detecting early-stage invasive breast disease, and interest in developing MR-guided biopsy techniques is on the rise. European researchers have reported positive experiences with open magnets, using technologies ranging from needle localization on supine patients to stereotactic localization using surface coils, perforated plates, breast coils, and even VAB under MRI guidance.
Three companies have developed stereotactic MRI breast biopsy devices, and two (Siemens Medical Solutions of Iselin, NJ, and Philips Medical Systems of Bothell, WA) have received FDA clearance. Fischer Imaging of Denver is readying a system for FDA review.
Other R&D efforts are focused on exploring the therapeutic margins of breast biopsy. Minimally invasive stereotactic laser therapy could be an effective treatment for some occult breast tumors identified on mammograms, according to preliminary research at St. Luke’s Medical Center in Chicago.
Another futuristic procedure, optically guided biopsy, could one day obviate traditional approaches to tissue assessment. Researchers in Barcelona have developed a high-speed technique that evaluates how light is scattered by cancerous tissue. Instead of waiting for histologic analysis following surgery, an optical biopsy would determine almost immediately if cancerous cells are present.
By Deborah R. Dakins
AuntMinnie.com contributing writer
May 16, 2002
Related Reading
Four biopsy passes accurate in assessing cancer grade, February 5, 2002
Stereotactic breast biopsy proves accurate for benign breast lesions, November 27, 2001
Vacuum-assisted breast biopsy less costly than needle-localized method, May 23, 2001
Practice makes perfect when it comes to stereotactic breast biopsy, May 5, 2001
References
Calcifications highly suggestive of malignancy: Comparison of breast biopsy methods, AJR, July 2001, Vol.177:1, pp. 165-172.
Learning curve for stereotactic breast biopsy: How many cases are enough?, AJR, March 2001, Vol.176:3, pp. 721-727.
Cost-effectiveness of stereotactic 11-gauge directional vacuum-assisted breast biopsy, AJR, July, 2000, Vol.175:1, pp. 53-58.
Full disclosure of breast biopsy options, AJR, April 2002, Vol.178:4, pp. 1029-1030.
Percutaneous imaging-guided core breast biopsy: Five years' experience in a community hospital, AJR, September 2001, Vol.177:3, pp. 559-564.
Copyright © 2002 AuntMinnie.com