The growth of radiology-focused breast health centers may be prodding radiologists into territory they have long avoided: the evaluation and management (E&M) of patients.
That's the prediction of Gerald Kolb, president of Breast Health Management, a consulting firm in Bend, OR. Kolb spoke at the 2002 National Consortium of Breast Centers conference in Las Vegas, and provided tips on how breast centers can set up and bill for E&M services.
Kolb said that increased coding for evaluation and management services by radiology-focused breast centers reflects a change in the way patients are -- and perhaps should be -- treated.
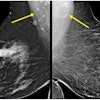
"Radiologists in active breast practices for the last 10 years have been doing what surgeons did before," Kolb said. "Nonpalpable lesions are being worked up by radiologists, and they are entitled to reimbursement for the evaluation and management of these patients."
In contrast, a diagnostic mammogram performed on a patient with a palpable lesion who has been referred for the study by her surgeon would not be an appropriate case for radiology E&M codes, Kolb wrote in materials accompanying his presentation.
The clinical breast radiologist should also be receiving "open" referrals, where the patient is referred for "diagnostic mammography, ultrasound, biopsy, and such other tests or procedures as may be necessary to appropriately diagnose the patient’s condition," Kolb wrote. "This kind of referral both documents the request that the breast radiologist manage the diagnostic process, and provides latitude with respect to the procedures that may be performed without seeking a further referral."
The components of evaluation and management of a patient include the taking of a medical history, examination of the patient, medical decision-making, counseling of the patient, coordination of care, the nature of the activities, and the time spent on those activities.
Time may be the critical element in determining whether an E&M reimbursement request should be coded at a higher level, Kolb said. He noted that coding Schedule C and Schedule D provide time approximations that may be used.
"When the consultation with the patient or her family, or the process of coordinating the care for the patient, becomes the dominant aspect of the encounter (e.g., accounts for over 50%), then time, if documented, will control the level of coding," according to Kolb.
Kolb recommended that radiology-focused breast practices consult with their breast surgery colleagues on how best to document time spent on evaluation and management. Kolb also cautioned that radiologists should never use Level 1 codes for E&M, as other physicians use such codes only for nurse time with a patient.
Specific evaluation and management codes cited by Kolb include:
- 99242, which would apply to an initial consultation in a Level 2 diagnostic appointment resolved with a mammographic and/or ultrasound examination.
- 99243, for the initial consultation in a Level 3 diagnostic appointment resolved with biopsy examination.
- 99212, covering a visit by an established patient in a follow-up appointment regarding biopsy results.
"The biggest mistake you can do is to bill for E&M without documentation and justification," Kolb cautioned. "Many private payers are going to push back on these."
That also means not billing E&M for radiologists who don’t want to take on that role.
"The physician needs to be prepared to look the patient in the eye and talk to them," Kolb said. "This is not money for nothing, it’s money for effort. In many cases, that effort is already being expended; in other places you may decide, ‘That’s what we should be doing.’"
Indeed, centers that rethink their practices in terms of evaluation and management may well improve the care they provide, Kolb suggested.
The move toward evaluation and management may also benefit a center’s bottom line. Kolb projected that appropriate billing of E&M in a hospital-based breast center can increase professional reimbursement by 30% and technical reimbursement by 10%. In a private breast center, E&M coding can increase reimbursement by 12%, he said.
By Tracie L. ThompsonAuntMinnie.com contributing writer
March 26, 2002
Related Reading
New year brings new coding and bundling changes, January 18, 2002
Detailed documentation delivers dollars and sense, July 31, 2002
Point-of-service coding ties payment to treatment, February 5, 2001
Offensive strategy may be mammographers’ best bet in reimbursement war, October 9, 2000
Copyright © 2002 AuntMinnie.com