Experience has always been the best teacher when it comes to virtual colonoscopy, and the radiologists at New York University Medical Center in New York City have learned much in seven years of performing the exam.
In a talk at the 2003 International Symposium on Multidetector-Row CT, NYU virtual colonoscopy veteran Dr. Michael Macari discussed what has worked and what hasn't, as seen through the prism of hundreds of patients and continuously evolving technology. Stanford University of Stanford, CA, hosted the symposium.
First, and notwithstanding promises of a prepless future, "I think in 2003 a clean, distended, dry colon is absolutely essential for performing virtual colonoscopy or CT colonography," Macari said. A good prep facilitates interpretation of the examination, and helps radiologists distinguish among the various types of filling defects.
Getting there means choosing one of several commercial bowel-cleansing preparations, the most common being a polyethylene glycol solution (Golytely, Braintree Laboratories, Braintree, MA). Safe and effective for all kinds of patients, this cocktail nevertheless has two key drawbacks, Macari said. First, it requires patients to drink a full gallon of liquid the day before the exam. Second, it can leave a lot of residual fluid in the bowel, complicating interpretation and potentially obscuring some lesions.
Turning the patient from supine to prone during acquisition is essential for redistributing the intraluminal gas and the residual fluid, and for determining if a suspected lesion is mobile and therefore stool, Macari said. But even so, excessive fluid keeps some studies unreadable.
"From time to time using the Golytely preparation there will be so much residual fluid that you can turn the patient supine and prone and not (succeed) in evaluating the entire colonic mucosa, Macari said. In fact, it's one of the key reasons why some advocate the use of intravenous contrast in virtual colonoscopy -- to highlight lesions that might otherwise be obscured.
"That said, we do use the...polyethylene glycol preparation for patients who have significant renal insufficiency or cardiac disease, because this preparation is neither absorbed nor secreted," Macari said. "It doesn't result in fluid shifts or hypernatremia ... so it is the bowel preparation to use in rather sick patients," he said.
For patients without such contraindications, the preferred prep choices are the phospha-soda kits (C.B. Fleet Company, Lynchburg, VA) or a magnesium citrate oral solution (Lo-So, EZ-EM, Lake Success, NY). These mixtures leave less residual fluid, come with written patient instructions, and can be picked up at the pharmacy, Macari said.
Regardless of the prep, however, some 2%-3% of preparations fail to clean the colon sufficiently to interpret the exam. Macari recommended reading the data to look for whatever clinically significant lesions might be visible, then asking the patient to redo the prep and come back.
There is much discussion about barium fecal-tagging agents as well, he said, but predicted that these will not come into widespread use until digital subtraction software has advanced to the point where prepless virtual colonoscopy is practical.
Throughout the virtual colonoscopy process, patients generate a lot of questions for the provider, Macari said. They want to know what to do, what to expect, and what drugs they can continue taking. As a result, a knowledgeable person should be available to take patient phone calls, else the radiologist winds up answering a lot of questions, he said.
Once patients have been prepped, room air or CO2 insufflation begins by inserting a catheter a few inches into the rectum. Macari said his group favors standard 5 1/2 mm catheters over balloon catheters. There is even a jumbo 15 1/2-mm catheter designed specifically for virtual colonoscopy, he said, but it has not been a hit with patients.
"Most people, even in New York, don't like these," Macari said.
A better option is to insert a 5 1/2-mm catheter and ask the patient to keep the buttocks tight to prevent air from escaping. At the same time, balloon catheters do have their place in some elderly or frail patients, and in others with poor sphincter control, Macari added.
Room air or CO2
"We traditionally used room air," Macari said. "It's quick, it's very easy, and the techs like it because we get the patients on and off (the table) in no time." But since a few patients have complained of post-exam cramps, the group has recently begun evaluating CO2, which can be insufflated either manually or electronically.
Preliminary research has shown that CO2 is absorbed through the colonic mucosa and excreted through the lungs, minimizing gaseous distension of the colon and preventing post-exam cramping. One study found that two minutes after the colon exam, half of the CO2 had been absorbed. "It does cost money, and it is a bit inconvenient, but there is potentially a role for CO2," Macari said.
The importance of having enough restrooms cannot be overstated, he said, and there are times when the group's single bathroom proved woefully inadequate.
"One day they scheduled three virtual colonoscopies in the morning," he said. "They all came in, they all had to use the bathroom, we filled them up with gas and they had to go back...it was really a big mess."
CT acquisition
In 1997, when the radiologists first started performing virtual colonoscopy, they used a single-slice spiral scanner to acquire 5-mm-thick sections at a pitch of 2, at 120 kVp and 150 mAs, resulting in a CTDI of 6.8 mGy. The technique yielded relatively poor axial resolution, Macari said.
The current four-slice scan protocol includes 4 x 1-mm collimation, 120 kVp, and effective mAs of 35, kept low with the aid of Siemens' CareDose tube current modulation, which adjusts tube current during the scan and matches the radiation dose to patient size. The total exam dose has been reduced to 4 mSv for male patients and 6 mSv for female patients, comparing very favorably with background radiation in New York City of a little over 3 mSv per year, he said.
The group has also installed a 16-slice scanner (Somatom Sensation 16, Siemens Medical Solutions, Malvern, PA). For most virtual colonoscopy studies the group acquires 16 x 1.5-mm-thick sections, reconstructing 2-mm-thick sections overlapping every 1 mm. The entire scan can be performed in nine seconds, yielding 900 images, and a radiation dose slightly lower than that of the four-slice machine.
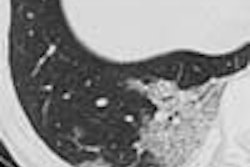
With minimal mAs, "we maintain a very good ability to differentiate folds from polyps from fecal material, because with high-contrast imaging you really don't need low noise," Macari said. "You do not need beautiful images for a (diagnostic) examination. With vascular studies, colonography studies, and kidney stones you can go for lower exposure." Thin-section overlapping reconstruction has improved the specificity of the group's findings, he said.
The group relies primarily on sagittal, axial, and coronal 2-D views, as well as multiplanar reconstructions and 3-D endoscopic views for problem-solving.
"We also need multiple window and level settings to differentiate polyps, fecal material, and (haustral) folds," he said. Three-dimensional imaging allows for differentiation of smooth from geometric morphology. "If you see something...that has geometric, angular borders, then you know this is residual fecal material -- polyps do not grow like this," he said.
The radiologist should maintain an awareness of the clinical significance of the lesions he is looking for, expressed in terms of its histology, morphology, and size. As for morphology, it cannot generally be determined in CT except in the case of lipomas, which are round, harmless, and occur in about 1% of patients, Macari said. Pedunculated lesions tend to have more benign histology than sessile polyps.
As in any type of imaging, the more a radiologist understands about what he is looking for, the better he can interpret what he is finding.
"While 90%...of colon cancers develop from the adenoma-carcinoma sequence we all learned in medical school...the vast majority of these tubular adenomas never develop the mutations to become a tubular villous adenoma or an invasive cancer," Macari said. "And those that do grow very slowly -- I'm talking 10 to 15 years. So if we could develop an algorithm for what we see in virtual colonoscopy, we can come up with a screening or surveillance interval."
One of the group's VC studies produced slightly higher sensitivity than conventional colonoscopy for the detection of lesions 10 mm and larger, he said. In one case, that meant sending a patient with a 14-mm lesion in the splenic flexure back to the endoscopist for another look. "If you're missing these you should not be doing virtual colonoscopy," he said. On the other hand, deciding what to do with lesions 5 mm and smaller is a little trickier.
"There are a number of different places across the country that are teaching people to interpret these examinations," Macari said. "If you're really serious about doing this, I think you should go to one."
By Eric BarnesAuntMinnie.com staff writer
July 25, 2003
Related Reading
Electronic virtual colonoscopy tutor emphasizes spectrum of abnormalities, May 13, 2003
Multislice CT may improve virtual colonoscopy results, May 2, 2003
Electronic CO2 insufflation beats air in virtual colonoscopy, March 12, 2003
Thin slices, narrow collimation rule in virtual colonoscopy study, March 8, 2003
Workflow issues key in virtual colonoscopy, January 15, 2003
Copyright © 2003 AuntMinnie.com