Investigations continue into the role and relevancy of ultrasound for the evaluation of breast cancer. Two recent studies took a closer look at sonography’s ability to spot missed abnormalities, either alone or when used in conjunction with traditional mammography.
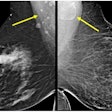
First, a team from New York University School of Medicine in New York City and Massachusetts General Hospital (MGH) in Boston studied the specificity of mammography and ultrasound (US) in the evaluation of palpable breast abnormalities. Specifically, they retrospectively reviewed the number of patients who still developed breast cancer despite combined negative findings with both modalities.
"Often, both mammography and US fail to demonstrate an abnormality...It was our anecdotal impression that the likelihood of cancer is low when both examination findings are negative," wrote Dr. Linda Moy and colleagues in Radiology Online (August 26, 2002).
Records for 829 women who had undergone mammography and ultrasound at MGH between January 1995 and December 1998 were included in this study. In these patients who were referred with a clinically palpable abnormality, the combined imaging findings were negative. The results were then compared to pathological information based on breast biopsies. The majority of the patients were available for a two-year follow-up.
Mammograms were acquired with one of three units (Senographe DMR or 800T, GE Medical Systems, Waukesha, WI; Contour, Bennett X-Ray; MAM-CP, Continental X-Ray). The exam consisted of at least the conventional two-view mediolateral oblique and craniocaudal projections of each breast.
Focused, real-time ultrasound exams were performed with either a 10-MHz transducer or an 11-MHz transducer (Logiq 400 MD, GE Medical Systems). The patient was in the supine position with the ipsilateral arm raised above the head.
"The criteria for true-negative findings included a benign result from biopsy of a palpable abnormality or a minimum of 2 years of negative follow-up results after the initial studies, and no evidence of tumor as per the State Cancer Registry," the authors wrote.
If the biopsy was positive within 2 years of the combined imaging studies, then the finding was deemed a false negative, they added.
Out of the 829 women, 58% had dense breast tissue, 12% had a family history of breast cancer, and 10% had a history of prior benign biopsy results.
Follow-up for at least two years was available for 233 patients. Of these, 97% were classified as true negatives. Eighty-three percent had benign biopsy results based on fibrocystic changes.
Despite combined negative mammographic and sonographic results, six patients were diagnosed with breast cancer in the area of the palpable abnormality, the group reported.
"We reviewed these patients’ mammograms," they said. "All patients...had heterogeneously dense breast tissue at mammography. In five patients, a focal abnormality could not be identified, even in retrospect. In one patient, a subtle mass on the mammogram may have been present."
The pathologic findings were invasive ductal carcinoma, pure ductal cacinoma in situ (DCIS), invasive lobular carcinoma, and invasive ductal carcinoma with associated DCIS.
The authors noted that "no breast cancers were found among women with fatty breast tissue compared with those with dense breasts. We suspect that if the tissues are fat at mammography, ultrasound has little to offer...."
They concluded that while a negative mammogram and sonogram cannot exclude breast cancer, the likelihood of malignancy is very low (2.6%-2.7%). The percentage rises to 3.8% if the patient has radiographically dense breast tissue.
Bilateral whole-breast ultrasound
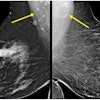
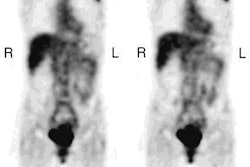
In a second Radiology study, Dr. Woo Kyung Moon and colleagues from Seoul National University in Korea evaluated the performance of preoperative bilateral whole-breast sonography in detecting additional multifocal, multicentric, and contralateral cancers.
"Of patients who are suspected of having unifocal breast cancer at clinical examination and mammography, 30%-63% will be found to have additional malignant foci in the ipsilateral breast and detailed serial slicing of the mastectomy specimen," the authors stated in their study’s introduction. "The purpose of our study was to evaluate the efficacy of preoperative bilateral whole-breast US...and the effect of US information on therapeutic decision" (Radiology, August 2002, Vol. 224:2, pp. 569-576).
Between January 1998 and January 2000, 201 patients underwent whole-breast ultrasound of the ipsilateral and contralateral breast before surgery. Their cancers were initially found on conventional film-screen mammography using the Senographe 600T system (GE Medical Systems). Routine mediolateral oblique and craniocaudal views were obtained.
Thirty percent of these patients had heterogeneously dense breasts; 35% had scattered fibroglandular tissues in fatty breasts; and 27% had extremely dense breasts.
In most of the women (157), the ultrasound exam was performed on a 10-12 MHz linear-array probe (HDI 3000 or HDI 5000, Philips Medical Systems North America, Bothell, WA). In 44 patients, a 13-MHz linear-array probe was used (Logiq 700, GE Medical Systems). The 20-minute scans were performed in the radial and antiradial planes, as well as in the longitudinal and transverse planes.
Additional foci from the index lesion (larger than 2 cm) were documented. Solid lesions were described according to their shape, orientation, echogenicity, echotexture, margins, and acoustic transmission. The lesions were then sampled for biopsy.
"In patients with additional cancers seen only at US, the mammograms were retrospectively analyzed...the failure to detect additional cancers were attributed to poor mammographic technique, interpretation error, anatomic area not included at routine mammography, and presence of obscuring dense parenchyma," the authors stated.
According to the results, in ipsilateral breasts, sonography depicted 97% of the foci of invasive cancer in 201 cases and 75% of the foci of DCIS in 69 cases. In comparison, mammography and physical exam (PE) found 86% of the foci of invasive cancer and 81% of the foci of DCIS. In the contralateral breast, ultrasound depicted 92% of 12 foci of invasive cancer and 57% of seven foci of DCIS. Mammography and PE found 50% of foci of invasive cancer and 71% of foci in DCIS.
"Overall, US depicted mammographically and clinically unsuspected multifocal and multicentric cancers in 14% of the patients and contralateral cancer in 4%," the authors said. Sonography alone detected 77 solid lesions, turning in a sensitivity of 100%, a specificity of 51%, a positive predictive value of 64%, and 100% negative predictive value.
Because ultrasound depicted more extensive disease than was previously determined on mammography, the therapeutic regimen was changed in 16% of the 201 patients, the authors wrote. In the majority of cases, mastectomy was performed instead of lumpectomy.
"The results of our study show that US can depict invasive and noninvasive breast carcinomas that are both mammographically and clinically occult, offering the potential for more accurate breast cancer staging and optimized treatment plans," they concluded.
The authors suggested that patients with large palpable tumors and those with dense breast parenchyma are the most likely to have additional tumors, and would therefore benefit the most from preoperative bilateral whole-breast ultrasound.
By Shalmali PalAuntMinnie.com staff writer
September 9, 2002
Related Reading
Sonographic findings in focal fibrocystic changes of the breast, May 29, 2002
THI ultrasound ups grayscale contrast in fatty breasts, May 10, 2002
High-resolution ultrasound may reduce need for breast biopsies, May 2, 2002
Copyright © 2002 AuntMinnie.com