LOS ANGELES - A new software program that co-registers nuclear medicine and CT or MR images has changed the way an Australian facility handles its nuclear pediatric imaging, particularly for patient follow-up.
Dr. Robert Howman-Giles Jr. from the Children’s Hospital at Westmead in Sydney shared his group’s work in a presentation Monday at the 2002 Society of Nuclear Medicine conference. His co-authors hailed from Westmead Hospital, also in Sydney.
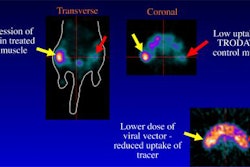
The software, designed in-house by physicist Dennys Lau of Children’s Hospital, used an algorithm that performs rigid image registration by maximizing mutual information (IDL version 5.0). Floating nuclear medicine images -- thallium, gallium, 123iodine-MIBG, and FDG-PET scans -- were matched with either CT or MRI target images, Howman-Giles said.
The group looked at the benefits of co-registration in the follow-up assessment of cancer patients for recurrence; initial diagnosis to localize metabolic areas for biopsy; and, in a few cases, therapy/ablation planning, he said.
For this study, 38 images were selected for coregistration. Six of these were specifically requested by the oncologists and had a significant impact on possible treatment plans.
The subjects ranged in age from 2 to 16 years. The following images were successfully coregistered with either CT or MR:
- 2 of 2 Tc-99m HMPAO of the brain (1 ictal, 1 stroke).
- 2 of 2 gallium scans of the neck (1 Hodgkin’s lymphoma, 1 nasopharyngeal carcinoma).
- 3 of 4 gallium scans of the chest with mediastinal pathology (2 lymphoma, 1 pulmonary metastases, 1 endocarditis).
- 8 gallium scans in the abdomen (2 sarcoma, 1 adrenocarcinoma, 3 hepatoblastoma, 1 nephroblastoma, 1 non-Hodgkin’s lymphoma).
- 4 123iodine MIBG scans (2 neuroblastoma, 1 phaeochromcytoma).
- 2 18F FDG-PET scans (hepatoblastoma).
- 2 of 3 thallium scans (3 Ewing’s sarcoma).
In one case, a 3-year-old child with nasopharengyeal carcinoma showed a large lesion on CT. Referring physicians needed to know the extent of the lesion in order to pinpoint a biopsy site. Coregistering the CT images with a gallium scan gave them that information, Howman-Giles said.
In another case, a 9-year-old who had been treated for hepatoblastoma three years prior was undergoing follow-up. Separate CT and gallium scans showed no abnormalities, but the patient still had a slowly rising AF (associative factor) protein level. Coregistration of CT and FDG-PET indicated a hot lesion posteriorly to the edge of the liver.
"This patient went to surgery, and using intraoperative ultrasound they were able to find this lesion. It was removed and his AFP (1-Fetoprotein) was normalized," Howman-Giles said. "In cases where it’s often quite difficult to exactly see and interpret the anatomical imaging, we find coregistration to be particularly useful."
Coregistration failed when different patient positioning was used for different modalities; there was a limited amount of CT or MRI data; or the area of interest was obscured by the intensity of tracer uptake.
Howman-Giles said he does not believe coregistration is necessary for all patients, but the technique has proved beneficial in pediatric oncology patients. The ability to coregister images is now offered routinely at the Children’s Hospital.
A recent editorial by researchers from the Middlesex Hospital in London declared that "PET/CT has arrived.… It is a truly new imaging tool which will change not just the use of PET but also the use of CT. Nuclear medicine specialists will appreciate the potential of this technology and will need rapidly to acquire further skills in cross-sectional imaging" (European Journal of Nuclear Medicine and Molecular Imaging, June 2002, Vol.29:6, pp.719-720).
By Shalmali Pal
AuntMinnie.com staff writer
June 18, 2002
Related Reading
Swiss researchers optimize CT-PET scanning protocols, March 4, 2002
Copyright © 2002 AuntMinnie.com