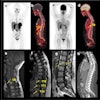
Restaging rectal cancer patients after surgery was more accurate with PET/CT than with PET alone, according to a study presented at last month's European Congress of Radiology in Vienna. Another presentation concluded that endoluminal ultrasound, despite limitations, has higher sensitivity for assessing local rectal tumor involvement than either MR or CT. And a study from Munich, Germany, found that multiplanar reconstructions are superior to standard axial reconstructions in assessing rectal tumor invasion.
Dr. Thomas Hany and colleagues from University Hospital in Zurich sought to assess the diagnostic impact of coregistered PET/CT imaging in patients with suspected primary or recurrent colorectal or anal carcinoma, compared to PET alone.
Sixty-five patients, including 43 who were being restaged following rectal cancer surgery, and 14 who were being evaluated preoperatively, underwent imaging on an in-line PET/CT system (Discovery LS, GE Medical Systems, Waukesha, WI), Hany said.
PET images were acquired following injection of 370 MBq of 18FDG. Patients also underwent an unenhanced, low-dose, four-row spiral CT protocol including 0.5-sec rotation, 140 kVp, and 80 mAs.
Two observers working independently analyzed PET images alone, and, four weeks later, coregistered PET/CT images, evaluating the images lesion-by-lesion to determine the correct staging. The results from both kinds of images were then correlated with information from clinical follow-up or histology when available.
According to the results, the primary tumor was detected by both observers in all 14 cases of preoperative assessment, both in PET/CT and PET alone. However, staging was more accurate and the diagnosis more confident with the addition of coregistered PET/CT.
The positive predictive value for the detection of recurrent cancer increased from an average of 71% to an average of 92.5% using PET alone and PET/CT, respectively. Moreover, there was substantially less over- or understaging using the combined modality (mean 10% versus 31.5% for PET alone), Hany said. Among 42 patients with recurrent colorectal carcinoma, there was "overstaging with PET alone in 5 patients," Hany said.
Interobserver variability for both observers was much lower with the combined modalities: kappa = 0.538 for PET and kappa=0.744 for PET/CT. In the correlation of data with histological findings, PET matched in 15/29 (52%) of patients, while PET/CT was correct in 25/29 (86%) of the cases.
"The increased level of certainty of the correct diagnosis is reflected in the decreased interobserver variability (p < 0.05 for both observers) when using PET/CT," Hany said. "This means that PET alone is good for staging rectal carcinoma, as we know. However, ... we believe PET/CT is more accurate than PET alone, especially for recurrent disease."
Multiplanar vs. axial reconstructions
In another ECR presentation, Dr. Christiane Kulinna from Ludwig-Maximilians University in Munich, Germany, examined the role of CT reconstruction methods in the detection and staging of colorectal carcinoma.
In the study, 55 patients with histology-proven colorectal cancer underwent multislice CT of the abdomen. Multislice CT images were acquired using a collimation of 1, pitch 6, and image reconstruction interval of 0.6 mm. Two kinds of reconstructions were then evaluated using:
- Multiplanar reconstructions (MPR) in the sagittal and coronal planes using 5-mm slice thickness and 4-mm increment.
- 5-mm slice width, standard axial reconstructions.
In double readings separated by a week's time, two observers blinded to the clinical and histological results evaluated the local T- and N-staging, first in the axial view, then using the multiplanar reconstructions.
According to the results, axial CT combined with MPR was 76% accurate for preoperative T-staging and 92% accurate for the detection of lymph node metastases, Kulinna said. In 10/55 patients, MPR -- in particular the sagittal slices -- provided more diagnostic information regarding the extent of tumor invasion. In the preoperative staging of patients with colorectal cancer, MPR was significantly better than axial images (p < 0.5%), she said.
Following the talk, an audience member asked if the results might not have been better using reconstruction slices thinner than 5 mm, but Kulinna said another study at her institution had found no diagnostically relevant differences between 1, 3, and 5-mm thick reconstructions. Some virtual colonoscopy studies have reached similar conclusions.
Endoluminal sonography beats MR, CT, but with limitations
Finally, a retrospective study presented at ECR found that, contrary to much of the existing literature, endoluminal ultrasonography (EUS) outperformed MRI and CT for staging rectal cancer and detecting lymph node involvement. To be sure, ultrasound has its limitations in rectal cancer assessment, but the modality was found to have high sensitivity and specificity in the retrospective meta-analysis.
Dr. Shandra Bipat, Dr. Jaap Stoker, and colleagues from the Academic Medical Center of the University of Amsterdam in the Netherlands searched the rectal cancer imaging literature between January 1985 and December 2001. They began by performing Medline searches of noninvasive rectal cancer imaging modalities using such keywords as "rectal neoplasm, ultrasonography, x-ray, CT..., MRI, specificity, false-negative," and "accuracy," Bipal said.
"The aim of our study was to perform a systematic review of the diagnostic accuracy of EUS, CT, and MRI in the T- and N-staging of rectal cancer," Bipat said. "With our search strategy we found 286 articles; 147 were relevant and 82 fulfilled all of our selection criteria."
To be included, a study needed a minimum sample size of 20 patients in a clinical cohort, histopathology as a reference standard, and sufficient data to construct 2 x 2 tables of the results, she added.
"We extracted 2 x 2 tables for T2, T3, T4, stages, and end-stage (disease)," she said. "There were no (staging) resources for the T1 stage so we did it separately.
Specificity and sensitivity were calculated from the 2 x 2 tables, and data analysis was performed according to a univariate random-effects model."
Overall sensitivity for assessing local invasion was 97% for EUS, compared with 79% for CT and 82% for MRI, she said. Specificity was 81%, 63%, and 72%, respectively.
For T1 staging, EUS had 71% sensitivity, compared with 56% sensitivity for MRI, Bipat said. For T2-stage disease, EUS' sensitivity was 93% (95% CI, 91%-95%), with specificity of 81% (95% CI, 77%-84%). In the T3 stage, EUS had 93% sensitivity (95% CI, 91-95%) and 81% specificity (95% CI, 77%-84%), with lower values for CT and MRI in stages 1-3. The addition of intravenous contrast did not improve the MRI results, Bipat noted.
In T4-stage disease, EUS' sensitivity was 85% (95% CI, 77%-90%) compared with 80% for CT and 74% for MRI. T4 specificity for the three modalities was 99% (95% CI, 98%-99%), 98% and 93%, respectively.
Still, ultrasound was less successful in detecting lymph node involvement, with sensitivity of 59% to 69%, and specificity of 75% to 80%, she said.
For T1-stage disease, EUS is the most accurate method compared to MRI and CT, while the modalities yield comparable sensitivity and specificity in end-stage disease, Bipat concluded. Still, "ultrasound has some major limitations" in staging rectal cancer inasmuch as it cannot readily detect stenotic lesions, lesions more than 10 cm from the anal verge, or distant lymph nodes, she said.
Following her talk, Bipat was asked why she thought ultrasound outperformed the other modalities, in contrast to the conclusions of other studies. She responded that the number of studies using MRI and CT, especially spiral CT, was limited. Moreover, the methodology did not permit the distinction of different MR acquisition techniques. And the preponderance of EUS studies might have resulted in an overestimation of EUS results, she said.
By Eric BarnesAuntMinnie.com staff writer
April 3, 2003
Related Reading
Study gives MRI edge over CT, US in rectal cancer staging, March 7, 2003
Racial gap in rectal cancer outcomes smaller in randomized trials, February 28, 2003
Reirradiation can be helpful in recurrent rectal carcinoma, September 27, 2002
For inoperable rectal cancer, radiation therapy alone may be enough, August 28, 2002
Copyright © 2003 AuntMinnie.com