CHICAGO - Previous lung cancer screening trials have established CT's ability to detect smaller, earlier-stage lung cancers in those who are screened vs. those who are not, raising hopes of a cure in at least some smokers and former smokers.
But the issue of screening remains problematic for several reasons. For one thing, CT detects a large number of nodules that are noncancerous, and CAD systems that might reduce the false-positive rate aren't ready for commercialization. For another, only 16% of smokers will develop the disease, leading to an enormous potential workload for CT screeners. Finally, the detection of central-compartment squamous-cell carcinomas is underrepresented in CT lung-cancer screening data.
In an effort to address these shortcomings, researchers from Vancouver General Hospital in BC, Canada, devised a protocol designed to prescreen subjects to find those at higher risk of lung cancer, while improving detection rates for the cancers CT tends to miss. Dr. John Mayo presented the results of his group's study at this week's RSNA lung screening sessions.
"We hypothesized that we could improve CT screening with the addition of computer-aided sputum cytology to identify those smokers who are at higher risk for lung cancer," Mayo said. "We also searched for central squamous-cell carcinomas within the airways that are not detectable using lung-CT screening protocols, using autofluorescence bronchoscopy."
The group examined 561 current and former smokers aged 50-70 who were recruited from the community, Mayo said. The subjects first underwent sputum sampling using high-frequency chest modulation and the induction of hypertonic saline. Induced sputum was assessed using a computer-assisted image analysis and classified as atypical or normal.
One hundred thirty-eight of 561 subjects had normal sputum while 423 had atypical sputum. Autofluorescence bronchoscopy was performed in 69 subjects with normal sputum, and in 308 of the atypical-sputum group. For fiscal and logistical reasons, autofluorescence bronchoscopy was used only in subjects with atypical sputum and/or suspicious nodules detected on CT, Mayo said.
"We went to a lot of effort to get our sputum," he said. "We used a sputum induction in a high-frequency chest oscillation (vest) (American Biosystems, St. Paul, MN). The subjects breathed nebulized isotonic saline and the sputum sample was collected. The sputum sample was then stained with a DNA-avid stain, and the volume and density of DNA in (thousands of) cells were determined." The computer categorized the DNA density as normal, intermediate or atypical.
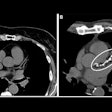
Low-dose spiral CT was performed in all subjects using either a single-slice (1.25 mm collimation, 120 kVp, 80 mAs, 0.5-second rotation, pitch 6) or comparable multislice scanning protocol. A thoracic radiologist reviewed the CT images on a workstation, recording each nodule detected.
White-light bronchoscopy and red-green autofluorescence bronchoscopy were performed in 377 subjects, Mayo said. More than 2,000 biopsies were performed in areas of abnormal autofluorescence.
"The results: 423 patients with sputum atypia had 13 primary lung cancers diagnosed within them; in 138 patients ... with normal sputum there were no cancers found, suggesting that this is a useful prescreening test," he said.
Seventy-seven percent of the cancers were stage 0 or I; 19% were stage 0 or II. Nine of 13 cancers were detected using spiral CT, with an average size of 16.8 mm, including six adenocarcinomas, one squamous cell carcinoma, one poorly differentiated small cell carcinoma, and one mixed small/large-cell carcinoma. Four cancers that were not seen on CT were detected in autofluorescence bronchoscopy, including three squamous-cell carcinomas in situ that were not visible on CT even in retrospect and one stage-I squamous-cell carcinoma.
The 21% false-positive rate in CT included noncalcified nodules and enlarged lymph nodes. Using all three screening methods the lung cancer prevalence was 3% in subjects with abnormal sputum, and 2.3% for the cohort overall. Eliminating the autofluroescence bronchoscopy as well as sputum cytology yielded an overall 1.6% prevalence of lung cancer.
"In conclusion, we believe that to increase the efficacy and accuracy of lung cancer screening, it may be useful to screen sputum cells and do computer-assisted sputum analysis," and to screen patients with abnormal sputum using both CT and autofluorescence bronchoscopy, Mayo said.
The cost of the added procedures is a drawback, but it will almost certainly drop as the technology develops further, he said.
By Eric Barnes
AuntMinnie.com
staff writer
December
2, 2002
Related Reading
Why CT lung cancer screening will (and won't) work, November 11, 2002
Copyright © 2002 AuntMinnie.com