Radiation therapy for the treatment of breast cancer significantly increases the incidence of major complications for women having implant-based breast reconstruction, according to new research published in the April issue of Plastic and Reconstructive Surgery.
However, based on a study of nearly 200 women, 80% who experienced complications as a result of radiation exposure during two-stage implant-based breast reconstruction following a mastectomy eventually attained success with either implants or autogenous tissue.
Radiation administered as treatment for breast cancer causes tissue damage that increases the risk of complications of breast reconstruction. In general, the use of autogenous tissue is recommended for patients who have undergone radiation therapy, but this type of reconstruction requires more extensive surgery, has a longer recovery time, and may cause greater comorbidities (Plastic Recon Surg, 2012, Vol. 129:4, pp. 817-823).
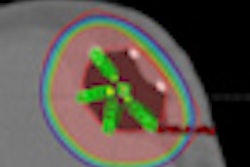
By comparison, implant-based reconstruction is a faster process. In two-stage reconstruction, a submuscular tissue expander is placed immediately following a mastectomy to increase the amount of the patient's own skin available for reconstruction. For the majority of patients, tissue expansions take place on a weekly basis starting three to four weeks following surgery. Several months later, the reconstruction is completed using the additional skin and breast implants filled with saline or silicone gel. In this study, for patients who had undergone radiotherapy treatment, this second stage was not performed for at least six months following radiation exposure (50 Gy to the ipsilateral chest wall in 25 2-Gy fractions).
A research team led by Dr. Kant Y. K. Lin, a plastic surgeon specializing in breast reconstruction at the University of Virginia in Charlottesville, conducted a retrospective outcomes study to determine if radiation-damaged soft tissues can be relied upon and used in two-stage implant-based reconstruction, especially if tissue expansion is to be employed. The success of this procedure is dependent on the malleability, durability, and, ultimately, long-term stability of the soft-tissue envelope used to cover the implant.
They retrospectively evaluated the outcomes of 267 breasts reconstructed in 194 patients over a 10-year period from January 2000 to December 2009. Thirty-eight percent of the patients had bilateral reconstruction.
The majority of patients (representing 82% of the breast reconstructions) did not require radiation therapy. However, the breasts of 32 patients (12%) were irradiated before mastectomy, and 17 breasts (6%) were irradiated after mastectomy and first-stage reconstruction.
Major reoperative complications following reconstruction occurred at a significantly higher rate for women who had radiotherapy treatments. The complication rate was 13.8% for breasts that had no radiation exposure, whereas it was 43.8% for breasts exposed to radiation before surgery, and 41.2% for those exposed after surgery.
The most common complication in both radiation groups was wound dehiscence. Twenty-two percent of women undergoing radiation had problems relating to wound healing, but only 2% experienced this among the women not treated with radiation. All of the women in the 2% group were smokers.
Problems with the tissue expander occurred with 19% of the breasts. However, the overall risk of major complications was about six times higher in women who received the radiotherapy.
The researchers evaluated age, body mass index (BMI), expander volume, whether patients underwent chemotherapy, and whether they had a history of diabetes or active smoking within 12 months of the date of surgery. Risk of major complications proved to be more than three times higher for smokers.
Noting that the rate of complications leading to repeat surgery for women who have undergone radiation therapy was prohibitively high, the authors suggested that the study provides important new data to help balance the risks and benefits of implant-based breast reconstruction when radiation therapy is also a part of treatment.