The American College of Radiology (ACR) has published a summary of its updated evidence-based guidelines for external-beam radiation therapy (EBRT) treatment planning for clinically localized prostate cancer in the April issue of the Journal of the American College of Radiology.
Guidelines for the ACR Appropriateness Criteria are reviewed and updated every two years. The guideline development was undertaken by a multidisciplinary panel that included an analysis of current medical literature from peer-review journals. It also included use of a consensus methodology to rate the appropriateness of imaging and treatment procedures, according to lead author Dr. May Abdel-Wahab, PhD, a radiation oncologist at the Taussig Comprehensive Cancer Center at the Cleveland Clinic in Ohio (JACR, 2012, Vol. 9:4, pp. 233-238).
The guidelines recommend that CT exams be used for simulation of patients with prostate cancer, but note that because CT images overestimate the size of the prostate gland by approximately 27% to 32%, and because the delineation of both the prostate and the seminal vesicles may be more accurate by MRI, this should be considered to aid in volume determination.
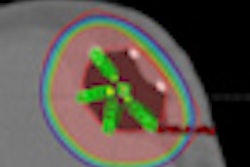
The committee stated that when MRI simulation was used instead of CT-based simulation for treatment planning, the penile bulb and corpora cavernosa had better sparing when intensity-modulated radiotherapy treatment (IMRT) was prescribed. Whether sparing of erectile tissues with MRI-based radiation treatment will lead to better sexual outcomes for patients remains unknown, nor is there knowledge of whether this could compromise long-term tumor control.
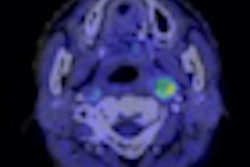
Dynamic contrast-enhanced (DCE) MRI can allow better targeting of tumors, including areas of extracapsular extension or capsular penetration, seminal vesicle invasion, and neurovascular bundle involvement. It also may allow targeting of dominant tumor nodules for a boost.
However, disadvantages of this type of exam include CT-MRI fusion uncertainties, treatment planning warping, and a loss of radiographic density information for calculating radiation doses and reconstructing digital radiographs for treatment verification. Also, the availability of DCE-MRI is limited, and because of this, hospitals may not have this exam option to offer patients.
The updated guidelines also recommend the use of daily localization, using techniques that require smaller margins. Intensity modulation may also be beneficial, with 3D blocks used in lieu of IMRT if the latter is not available.