An MRI-based radiomics model can help predict breast cancer chemotherapy response, researchers have reported.
The study results could help clinicians determine the best care for women with the disease, wrote a team led by Jie Hou, PhD, of Hangzhou Medical College in Hangzhou, Zhejiang Province, China. The work was published July 15 in the International Journal of Cancer.
"[Our findings establish] an MRI-based biologically interpretable pCR [pathological complete response] predictive tool, which has the potential to individually guide clinical decision-making," the group noted.
Breast cancer is the second most common cause of cancer-related mortality around the world, and chemotherapy is the first-line treatment, the investigators explained. Early prediction of pCR status after neoadjuvant chemotherapy can help clinicians tailor treatment and make effective prognoses in breast cancer patients, the investigators explained.
"Patients who achieved … [pCR] often exhibit a longer disease-free survival, [but] only 19% to 30% achieve pCR at the current juncture," they wrote. "Therefore, as an early clinical endpoint for long-term survival, reliable prediction of pCR would substantially advance the development and improvement of personalized treatments."
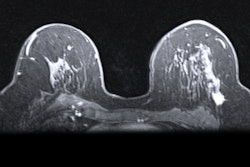
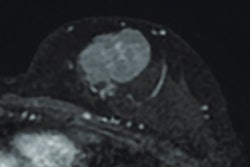
MRI helps clinicians evaluate changes in tumor morphology, cell density, and vascular distribution after chemotherapy, but there remain key differences between MRI evaluation and pathological standards for pCR. That's where radiomics could help, Hou and colleagues wrote.
"Radiomics can … combine clinical information, molecular characteristics, and histopathology to enhance the accuracy of disease diagnosis and prognosis, making medical imaging more closely aligned with personalized medicine," they noted.
The group sought to create and test a radiomics approach based on DCE-MRI and clinicopathological information to predict pCR and assess different disease-free survival risks after chemotherapy.
The study included 843 breast cancer patients recruited from three medical centers; the total study population was divided into training (n = 385), internal (n = 165), and external (n = 293) validation cohorts. The researchers extracted 944 radiomics features from tumors and 4 mm peritumor regions on dynamic contrast-enhanced (DCE)-MRI images and also took into account clinical-pathological factors such as age, menopausal status, tumor site, estrogen receptor, progesterone receptor, HER2, and histological grading. Finally, Hou and colleagues set the following radiographic characteristics for comparing radiologist performance to the prediction model: tumor edge, tumor morphology, and enhancement mode.
The group reported that the pCR-related hybrid model outperformed both junior and senior radiologists as assessed by the area under the receiver operating curve (AUC).
Comparison of AI model to radiologist readers for predicting breast cancer patient response to chemotherapy | |||
Measure | Junior radiologist | Senior radiologist | pCR-related hybrid model |
| AUC (range) | 0.62 to 0.76 | 0.64 to 0.77 | 0.8 to 0.89 |
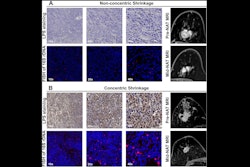
The team also found that radiogenomics analysis further showed that predicted pCR was associated with immune and inflammatory pathways, while no-pCR was associated with cell proliferation and tumor invasion processes.
The takeaway? An MRI-based, biologically interpretable pCR predictive tool such as this one could "potentially be used to guide individualized clinical decision making," the researchers concluded.
The complete study can be found here.