Delaying initial radioactive iodine-131 (I-131) therapy more than 180 days after total thyroidectomy may result in poor survival for thyroid carcinoma patients, according to a study published in the May issue of the Journal of Nuclear Medicine.
Japanese researchers found that when initial radioactive iodine therapy was delayed more than 180 days, the risk of death was 4.22 times higher than among thyroid cancer patients who received initial therapy within 180 days. The lead author of the study is Dr. Tatsuya Higashi from Shiga Medical Center Research Institute (JNM, Vol. 52:5, pp. 683-689).
The retrospective study initially reviewed 413 patients with thyroid carcinoma who received total thyroidectomy between January 1997 and June 2009. The researchers included patients with cases of thyroid carcinoma or other variants of thyroid carcinoma at the time of total thyroidectomy. In addition, patients were to have received at least one radioactive iodine treatment during the study's time frame.
The study also required clinical follow-up for more than one year, and that the patient be younger than 45 years old with distant metastases at the time of thyroidectomy or older than 45 years with at least stage III thyroid carcinoma at the time of thyroidectomy.
Patients were excluded from the study if they had pathologically confirmed anaplastic carcinoma, undifferentiated carcinoma, medullary carcinoma, or malignant lymphoma at the time of total thyroidectomy, or if their clinical follow-up had been less than one year, among other factors.
The final cohort included 198 patients with an average interval between total thyroidectomy and initial radioactive iodine therapy of 2.59 years (range, 844-1,546 days). The researchers used patient records and clinical follow-up to confirm disease-specific survival, with the primary end point of survival as the date of death.
Patient medical records showed that 124 patients received total thyroidectomy at the time of initial thyroid carcinoma detection, with 59 (47%) receiving hemithyroidectomy or subtotal thyroidectomy, and then total thyroidectomy later in their course of treatment (average interval, 6.3 years). The interval was unknown in 15 of those 59 patients.
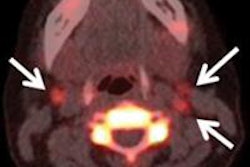
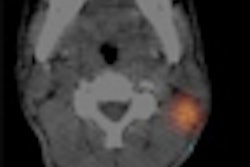
An average of three days after receiving I-131 orally, a standard whole-body exam was performed with a dual-head gamma camera.
A total of 67 patients had observation periods without therapy of 180 days or less, 20 has periods between 180 days and 365 days, and 11 had periods between one and two years. In addition, 13 patients had observation periods without therapy of two to three years, and 73 patients had observation periods without therapy of three years or more.
Clinical follow-up
Based on clinical follow-up, 31 patients died during the observation periods. Two patients who died from cachexia and respiratory failure due to lung metastases were excluded from the present study. Five patients who died for nondisease-specific reasons, including esophageal, gallbladder, and gastric cancer, were also excluded from the study.
The exclusions left 24 deceased patients (11 males and 13 females) for analysis. The reasons for death included 11 cases of respiratory failure due to lung metastases, six cases of uncontrollable brain metastases, three patients with massive hemoptysis from respiratory tract metastases, two cases of asphyxia related to a bulky neck mass, and one case each of cachexia due to multiple metastases and hemorrhagic cardiac tamponade due to direct invasion.
The average cumulative number of radioactive iodine therapies (RITs) for deceased patients was four, ranging from one to 26 treatments. On average, deceased patients had an initial RIT at age 62.5 years, which was significantly older than for the survivors. There were no deceased patients younger than 45 years old, with solely local disease, or with lymph node metastases at the time of initial RIT.
The average interval between total thyroidectomy and initial RIT in the deceased patients was 4.08 years, which was significantly longer than the 2.4-year interval in the survivors.
In addition, the age at initial RIT of patients older than 45 years showed a significantly high prognostic value, while an interval between total thyroidectomy and initial RIT of 180 days or more also showed significant prognostic value.
Researchers' conclusion
Based on the results, Higashi and colleagues concluded that the delay of initial RIT until more than 180 days after total thyroidectomy in thyroid carcinoma patients with metastases resulted in poor survival. "Performing initial RIT within 180 days after total thyroidectomy may improve survival in postoperative differentiated thyroid carcinoma patients with metastases," the authors wrote.
The authors cited several limitations of the retrospective study. They noted that by including only thyroid carcinoma patients treated by RIT, the results may come from a biased patient group.
In addition, the statistical analysis focused on clinical factors at the time of initial radioactive iodine therapy.
"RIT is usually performed multiple times during long periods in most patients, and these cumulative therapeutic effects may have a great impact on prognosis," the authors wrote. "Further research evaluating the cumulative therapeutic effects of RIT on prognostic value in differentiated thyroid carcinoma patients is needed."
Impact on public policy
The Japanese study is cited in another article in the May issue of JNM, regarding the U.S. Nuclear Regulatory Commission's (NRC) recommendation of outpatient treatment for patients receiving radioactive iodine after total or near-total thyroidectomy. Opponents of the policy are urging NRC to mandate overnight hospital stays to protect people from a perceived risk of radiation exposure.
Dr. Stanley Goldsmith, director of the division of nuclear medicine at NewYork-Presbyterian Hospital and Weill Cornell Medical College, cited the findings from Higashi et al as a reason to maintain the current NRC policy. If NRC were to require overnight stays, he asserted, a backlog could result and cause delays in the treatment of patients.
"There is ample evidence that I-131-treated patients can be released with prudent advice about potential exposure to others and without injury to family members, hotel workers, or the general public," Goldsmith wrote. "It is importantthat we continue to challenge unsubstantiated concerns that might interfere with patient access to I-131 and the adverse consequences that result from treatment delays."
SNM issued a joint statement with the American Thyroid Association, the Endocrine Society, and the American Association of Clinical Endocrinologists stating that existing scientific evidence shows current I-131 regulations are safe for patients, their families, and the public when radiation safety instructions are followed.