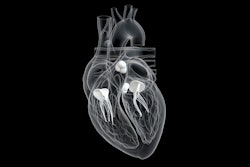
Coronary CT angiography (CCTA) helps predict risk of major adverse cardiac events in patients with non-ST segment elevation (NSTE) acute coronary syndrome (ACS) -- in part by its ability to quantify lipid-rich plaque, a study published August 22 in Radiology has found.
The research suggests that CCTA shows promise as an effective and less invasive tool than other forms of intravascular imaging for this purpose -- specifically invasive coronary angiography (ICA) -- wrote a team led by Zhong-Fei Lu, PhD, of Fuwai Hospital in Beijing, China.
"CCTA and ICA have equivalent ability to predict long-term risk through assessment of the severity and extent of obstructive coronary artery disease," the group noted. "Additionally, CCTA could be used to reduce the rates of ICA and has emerged as an important technique in the visualization of coronary plaque characteristics, allowing for a fast, noninvasive quantitative evaluation of plaque burden and composition."
Fatty plaques are associated with adverse cardiac events in patients with NSTE, and patients presenting with the condition are typically worked up with invasive coronary angiography (ICA). CCTA can better assess plaque composition than ICA, but its prognostic performance for this indication remains unclear.
To address the knowledge gap, Lu's team investigated whether there are quantitative variables on CCTA imaging that reflect lipid content in nonrevascularized plaques in individuals with NSTE ACS -- and whether these variables could help predict ensuing plaque-related major adverse cardiovascular events.
The study included 342 patients diagnosed with NSTE acute coronary syndrome and was conducted between November 2017 and January 2019. All participants underwent CCTA before invasive coronary angiography within a day of presenting with cardiac symptoms. Median follow-up for the participant cohort was four years.
The investigators found a nonrevascularized plaque-related major adverse cardiac event rate of 23.9%. They also found that higher lipid core burden (≥ 2.8%) was an independent predictor of higher risk of these events at the participant level (hazard ratio, 12.6, with 1 as reference) and that lipid core burden and volume was an independent predictor of higher risk of these events at the plaque level (hazard ratio, 12.1 and 11, respectively).
| CCTA findings in patients without and with nonrevascularized plaque-related major adverse cardiovascular events* | |||
| Variable | Overall | Cohort without nonrevascularized plaque-related major adverse cardiovascular events | Cohort with nonrevascularized plaque-related major adverse cardiovascular events |
| Participant level | |||
| Total plaque volume | 105.1 mm3 | 83.1 mm3 | 265.3 mm3 |
| Lipid core volume | 11.3 mm3 | 7.3 mm3 | 37.6 mm3 |
| Plaque burden | 37.1% | 33% | 46.5% |
| Lipid core burden | 5.6% | 3.8% | 12.8% |
| Plaque level | |||
| Total plaque volume | 53.7 mm3 | 48.1 mm3 | 101.2 mm3 |
| Lipid core volume | 3.6 mm3 | 2.7 mm3 | 18.3 mm3 |
| Plaque burden | 39.6% | 37.5% | 52.7% |
| Lipid core burden | 3.9% | 2.8% | 17.7% |
"Participants with a high lipid core burden [of more than 2.8%] were nearly 13 times more likely to develop nonrevascularized plaque-related major adverse cardiovascular events ... than participants with a lipid core burden of less than 2.8%," the team reported.
The study makes a significant contribution to the literature, but more research is needed, wrote Sina Tavakoli, MD, PhD, and Emrah Duman, MD, both of the University of Pittsburgh, in an accompanying commentary.
"To improve patient outcomes, further research and validation are necessary to assess the clinical utility and impact of a comprehensive approach to risk stratification and plaque characterization by combining systemic medical therapies with plaque-specific interventions," they wrote.
The complete study can be found here.