
Two new studies have examined the role of MRI and CT in breast cancer and subsequent metastatic disease. Radiologists in New York City took a closer look at the routine use of chest, abdomen, and pelvic CT -- to spot hepatic lesions -- in breast cancer patients. While CT pinpoints small lesions (1.5 cm or smaller), the features on CT imaging tend to be nonspecific. The authors asked if MRI should be used to differentiate benign and malign lesions in patients with indeterminate CT findings.
In the second study, Japanese researchers pitted MRI against multidetector-row CT (MDCT) for determining the lesion margins for surgical removal. They found that one modality was superior to the other.
Hepatic lesions
Women with breast cancer often have hepatic lesions that are too small to characterize with CT, the standard imaging modality used in these patients. So is it worthwhile for these women to undergo MRI to further characterize the lesions? No, according to a study out of the Memorial Sloan-Kettering Cancer Center in New York City.
"The reported incidence is at least one hepatic lesion too small to characterize in 29.4% of women without definite liver metastasis on CT," explained Dr. Stacey Patterson and colleagues. "Given that the overwhelming majority of such lesions are benign ... immediate further evaluation with MRI offers marginal benefit beyond peace of mind." Since the study was conducted, Patterson has moved on to Mount Sinai Hospital of Queens in New York City (American Journal of Roentgenology, August 2006, Vol. 187:2, pp. 307-312).
For this retrospective review, more than 5,000 women diagnosed with breast cancer between 2000 and 2003 at Sloan-Kettering were included. All MRI exams were done on 1.5-tesla scanners and the protocol included axial in-phase and opposed-phase T1-weighted gradient-echo images; axial fat-saturated fast spin-echo T2-weighted images; and dynamic multiphase gadolinium-enhanced axial T1-weighted gradient-echo images. CT scans were obtained on scanners with 7.0- to 7.5-mm collimation.
According to the results, 1.4% of the 5,440 women underwent MRI of the abdomen after initial diagnosis of breast cancer. Of those 76 patients, 50% had at least one hepatic lesion that was deemed too small to characterize on CT. The majority of these women (61%) had more than one lesion, including cysts and hemangiomas. In 21% of these patients, no lesion was found on MRI at the site that corresponded to at least one small hepatic lesion found on CT.
 |
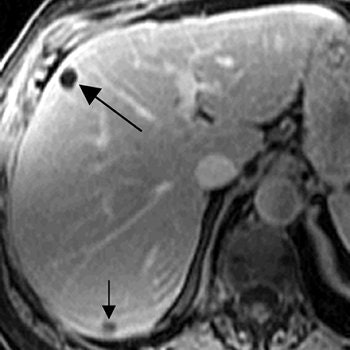
| A 71-year-old woman with invasive ductal carcinoma. Above, contrast-enhanced CT shows hepatic lesion (arrow) deemed too small to characterize. Below, contrast-enhanced T1-weighted MR image obtained 13 days after CT shows lesion (large arrow) in CT image is not enhanced, diagnostic of cyst. Lesion (small arrow) in posterior right lobe represents partial volume averaging of another cyst, which was evident in more caudal images (not shown). Patterson SA, Khalil HI, and Panicek DM, "MRI Evaluation of Small Hepatic Lesions in Women with Breast Cancer" (AJR 2006; 187:307-312). |
 |
Overall, only 5% of the hepatic lesions were considered malignant based on the MR study, the authors noted. The majority of lesions was benign or remained indeterminate. "Thus in 95% of the women ... the results of MRI did not alter medical management because therapy is not changed for benign or indeterminate liver lesions.... MRI is not warranted," they concluded.
A previous study has also recommended against liver imaging in patients with pathologically confirmed early-stage breast cancer because of a high false-positive rate and high cost. Another study voted against perioperative liver screening with ultrasound for patients without clinical signs of tumor spread (Archives of Surgery, May 1999, Vol. 134:5, pp. 551-553; Breast Cancer Research and Treatment, November 2003, Vol. 82:1, pp. 29-37).
On the other hand, a third study found that T2-weighted fast spin-echo contrast-enhanced MRI effectively characterized renal cysts of less than 5 mm. Patterson's group suggested that the study results may have differed because the lesions were particularly small and there was known history of breast cancer (Radiology, December 2001, Vol. 221:3, pp. 628-632).
The AJR authors stressed that their study was not designed to assess the accuracy of the two modalities, but instead to evaluate their actual clinical practice. While thinner sections CT may have been more useful for the initial look at these hepatic lesions, thinner slices would have been likely to contain even more lesions that defined characterization, they stated.
Intraductal cancer
The overall survival rate for women who undergo breast-conserving surgery is significantly lower when surgical margins are positive for tumor cells than with negative margins, and a positive surgical margin is generally the result of inadequate resection of the cancer's intraductal component, explained Dr. Akiko Shimauchi and colleagues from the Tohoku University Graduate School of Medicine in Sendai, Japan. Accurate preoperative diagnosis of the intraductal component is necessary to achieve a cancer-free surgical margin. Previous studies have evaluated MDCT and MRI in this setting, but these were done before current advances in CT technology, and often used two different patient populations.
"We compared the accuracy of MDCT and MRI for evaluating intraductal components of breast cancer in the same population," wrote Shimauchi, who is now at the University of Chicago in Illinois. "We propose that MRI is better than MDCT for evaluating tumors with ductal extension, especially those with relatively small intraductal components" (AJR, August 2006, Vol. 187:2, pp. 322-329).
This study included 69 patients who were diagnosed with breast cancer between 2000 and 2004, and who underwent breast-conserving surgery, as well as preoperative MDCT and MRI. CT exams were done with a collimation of 1.25 mm and a pitch of 6 (LightSpeed QX/i, GE Healthcare, Chalfont St. Giles, U.K). MR imaging was performed on a 1.5-tesla unit (Magnetom Vision, Siemens Medical Solutions, Malvern, PA). Patients were scanned in the prone position and the protocol included bilateral fat-saturated T1-weighted imaging and T2-weighted imaging. Dynamic contrast-enhanced studies in the sagittal plane were also done.
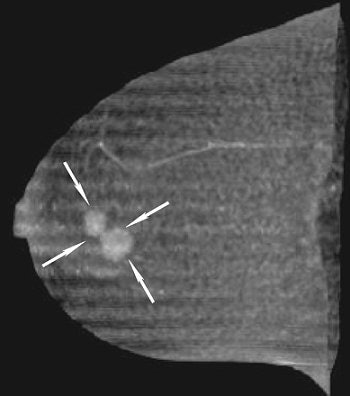 |
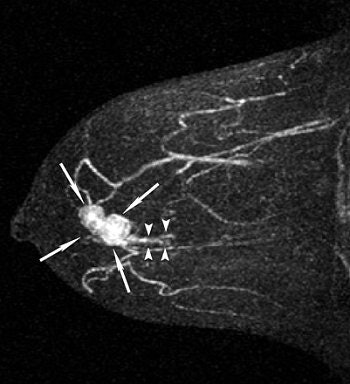
| A 43-year-old woman with invasive ductal carcinoma in right breast. Above, maximum intensity projection (MIP) image of MDCT images reveals location of main tumor (arrows) but not intraductal component. Below, MIP image of MRI reveals a clumped enhancement (arrowheads) distal to main tumor (arrows), which was suspected to be intraductal component. Intraductal component distal to main tumor was confirmed on histopathologic examination. Shimauchi A, Yamada T, Sato A, Takase K, Usami S, Ishida T, Moriya T, and Takahashi S, "Comparison of MDCT and MRI for Evaluating the Intraductal Component of Breast Cancer" (AJR 2006; 187:322-329). |
 |
Based on histopathology results, the majority of the tumors (63) were invasive ductal carcinoma and 44 of these had an intraductal component. Two radiologists reviewed the images in consensus, taking into consideration the distribution pattern of lesion enhancement and the morphologic typing of invasive tumors.
All 69 cases of invasive carcinoma were depicted on MDCT and MR images. The sensitivity of CT for detecting an intraductal component was 61%. Its specificity was 88% and the accuracy was 71%. In comparison, MR's sensitivity came in at 75%, its specificity at 88%, and its accuracy at 80%. In six patients, intraductal components were seen on MRI but not on CT. Both modalities missed intraductal components in 11 cases.
"There were no cases in which MDCT revealed an intraductal component that was undetectable with MRI," the authors stated. "The greater contrast obtained with MRI by using the subtraction technique probably contributed to the higher sensitivity of this method."
In terms of the morphologic typing of tumors, both modalities generally underestimated the length of the intraductal component. The correlation co-efficient between the length of the main tumor on MDCT and histopathology was 0.72 versus 0.70 for MRI. However, "underestimation of the length of the intraductal component by 15 mm or more was significantly less frequent with MRI than with MDCT," the group wrote.
Another drawback of CT is radiation exposure, although the modality does offer a faster scanning speed than MRI and is more widely available. Nevertheless, MRI proved to be the more precise exam and was less likely to underestimate the intraductal component. The authors pointed out that the latter is especially important as the intraductal components are used to determine the margin for surgical removal.
By Shalmali Pal
AuntMinnie.com staff writer
August 25, 2006
Related Reading
MRI accurately pinpoints common, benign liver lesions, May 27, 2006
Breast CT developers aim to 'revolutionize' mammography, December 20, 2005
Researchers make inroads with breast CT, gear up for clinical test, July 25, 2005
MRI after CT cuts need for liver biopsies in cancer patients, May 19, 2005
Copyright © 2006 AuntMinnie.com




















