The five-year survival rate for bronchogenic cancer is just 14%, and with some 169,500 new cases appearing each year in the U.S., researchers are eager to improve the odds of patients who are diagnosed with the disease.
In the September issue of Radiology Online, a group from the University of Colorado and the Denver VA Medical Center reported early results from a pilot CT lung screening trial designed to take advantage of the latest knowledge regarding the development of lung cancer, still the leading cause of cancer deaths in the U.S. The group's results suggest that a randomized and controlled multicenter trial could provide reliable information on whether CT screening reduces lung cancer deaths.
Several large trials undertaken in the 1970s and 1980s, at Johns Hopkins University in Baltimore, Memorial Sloan-Kettering in New York City, and the Mayo Clinic in Rochester, MN, failed to demonstrate that periodic chest x-ray and sputum analysis could reduce mortality, Dr. Kavita Garg and colleagues wrote (Radiology Online, September 19, 2002).
However, much has been learned about lung cancer since those trials were concluded. Notably, that long-term smokers with airflow obstruction secondary to chronic obstructive pulmonary disease have high incidence of lung cancer compared to similar smokers with no airflow obstruction.
"In addition, cytologic atypica detected in the expectorated sputum has been associated with a higher incidence of bronchial dysplasia and the development of lung cancer," they wrote. "On the basis of a combination of tobacco exposure history, presence of airflow obstruction at pulmonary function testing, and presence of sputum atypia, cohorts at high risk for lung cancer can be identified."
CT has improved too, of course, and has been shown in several studies to be superior to chest x-ray for the early detection of lung cancer. But while 85-95% of the lung cancers detected in the early Lung Cancer Action Project (ELCAP) and the Anti-Lung Cancer Association (ALCA) project were stage I and therefore potentially curable, the two studies were not designed to measure the effects of screening on mortality.
In an effort to fill the knowledge gap, the Colorado group is recruiting 400 high-risk individuals -- current or former smokers aged 50-80 with a cigarette smoking history of 30 or more pack years -- to participate in the randomized, controlled, low-dose CT lung screening trial.
The high-risk group (200) have diagnosed pulmonary airflow obstruction, and sputum cytologic analysis is performed at study entry and annually thereafter. The moderate-risk subjects (200) do not have symptoms of chronic obstructive pulmonary disease (COPD) in pulmonary function testing, do not use an inhaler, and do not have sputum cytological analysis performed at entry into the study, the authors wrote.
So far, 239 subjects have agreed to participate in the trial, where they are randomly chosen to either undergo CT screening or observation. Negative screening CT exams are repeated one year after the initial exam, and all current smokers are offered a referral to the VA's smoking cessation clinic, the article stated.
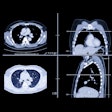
Baseline thoracic CT data are acquired over approximately 30 cm using a single-detector scanner (Picker 5000, Marconi Medical Systems, Cleveland, OH) using 120 kVp, 50 mA, 5-mm collimation and 3.5 mm reconstruction intervals.
The studies are read by a highly experienced board-certified chest radiologist, with routine review of many studies by a similarly qualified radiologist.
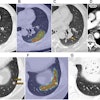
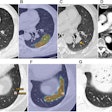
Nodules detected at baseline are evaluated according to the criteria used by Henschke et al (The Lancet, July 10, 1999, Vol. 354:9173, pp. 99-105). If noncalcified nodules are found, the subjects undergo contrast-enhanced diagnostic CT using 200 mA, 5-mm collimation, and 2:1 pitch. The field of view was the same as that used in the screening exam to facilitate comparison.
So far, 1-6 noncalcified nodules have been detected in 30/92 subjects (33%) who have undergone CT. Among those 30 subjects, 3 had a single noncalcified nodule 1 cm or larger, two of which were malignant. These included a 12-mm peripheral squamous cell carcinoma, and a 28-mm nodule consistent at biopsy with small-cell lung cancer. The remaining 27 subjects had nodules smaller than 5 mm, and follow-up in 16 has showed no change in size, the authors wrote.
No nodules were found in 65% (60) of the subjects, one subject had multiple granulomas, and one was found to have a metastasis from laryngeal cancer.
Among the first 92 exams, the authors noted a trend toward a significantly higher prevalence of nodules in the high-risk group compared with subjects of moderate risk (40% vs. 22% P=.07).
"Our results confirm a high degree of willingness by subjects ... to enroll in a randomized trial when the control arm of the study consists of only observation," the authors wrote, noting that 88% of the high-risk patients and 71% of the moderate risk patients were willing to participate in the ongoing study.
However, they added, "we are observing that it is not uncommon for them to delay their follow-up studies. Full compliance with not only the initial CT examination but also the recommended follow-up will be an important aspect of this ongoing feasibility study."
The study's limitations include a population of veterans with few women, and a small sample size to date. Mortality rates will only come with a longer period of time and a much larger sample size, they wrote.
"A multiinstitutional randomized controlled trial on a much larger scale is warranted to detect any effect of CT screening on mortality rate from lung cancer, and the results of this study suggest that such a trial could be conducted," they concluded.
By Eric BarnesAuntMinnie.com staff writer
October 10, 2002
Related Reading
In-line PET-CT system improves cancer diagnosis, October 10, 2002
CT, x-ray to face off in lung cancer screening megatrial, September 19, 2002
Spiral CT promising for lung cancer screening, August 2, 2002
US cancer rate falls but numbers set to rise, May 15, 2002
Copyright © 2002 AuntMinnie.com