If you're looking for a hot topic in molecular imaging, the "I's" may have it: The latest research indicates that iodine-131, generally considered the gold-standard thyroid cancer diagnosis, is less than perfect. In fact, a phenomenon called stunning can occur from the use of 131I, and the isotope may have a negative impact on treatment outcome.
As a result, investigators are turning to iodine-123 as a potential alternative. But as with most new treatment methods, there are still questions that need to be answered. Endocrine/thyroid and nuclear medicine specialists are actively debating the merits of 123I versus 131I for thyroid cancer diagnostic imaging.
The stunning issue
Dr. Stephen Gerard and associates from the San Francisco VA Medical Center in California have tackled what Gerard called the "10-year, ongoing controversy about the existence of stunning and the effect on 131I treatment outcome."
Stunning refers to the phenomenon in which the tissue is "killed" by the beta particles that 131I emits, explained Dr. Hee Myung Park from Indiana University in Indianapolis.
 |
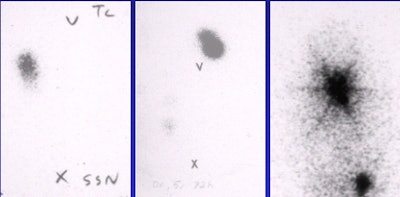
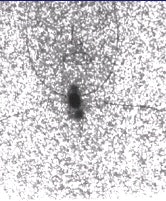
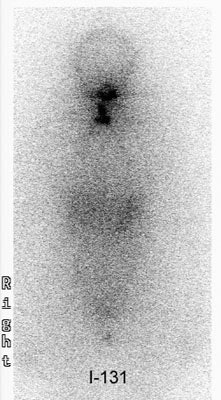
| Fifty-three-year-old male with papillary carcinoma who underwent total thyroidectomy. First post-operative scan with 5 mCi 131I at 72 hours. Two foci of remnant metastases are seen. |
 |
| Four weeks later, a scan with 100 mCi 131I at 72 hours was obtained. The stunned lesions failed to take up any of the therapy dose. |
 |
| At one-year follow-up on 5 mCi 131I scan at 72 hours, the same two lesions are present. Images courtesy of Dr. Hee Myung Park. |
The degree of stunning depends on the absorbed radiation dose. The effect of stunning may not be immediately apparent visually, and requires quantitative uptake calculation, he explained.
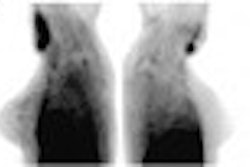
 |
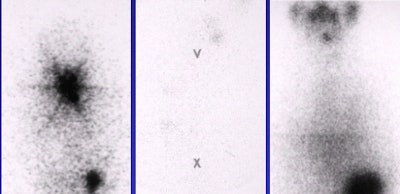
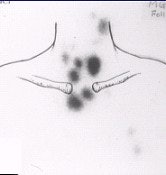
Above, an 131I diagnostic scan. Below, a post-therapeutic 131I scan. In these three patients who received 131I therapy the same day as the diagnostic scan, stunned thyroid lesions failed to take up any of the therapeutic dose. Images courtesy of Dr. Hee Myung Park.
 |
Park also said that the success rate of thyroid cancer ablation appears to diminish with higher 131I scanning doses. However, what constitutes a safe dose of 131I 131 -- 3, 2, or 1 mCi -- is still not known, Park said.
And 123I is not without its own stunning properties. Dr. Tom Hilditch and co-authors from the Western Infirmary in Glasgow wrote about the self-stunning effects of 123I in the European Journal of Nuclear Medicine and Molecular Imaging.
Reduced uptake of the therapeutic administration ( P<0.001) was observed in all 26 patients given diagnostic 131I, with a median value of 32.8% of the uptake in the diagnostic study. In the patients given diagnostic 123I, reduced uptake of the ablative radioiodine was observed in 15 of the 16 patients ( P<0.001), and the overall median value was 58.8% of the diagnostic uptake, they reported.
"The stunning observed in the group given 123I was significantly less ( P<0.001) than in the group given 131I," they wrote. "The stunning observed using 123I could not be explained by errors in the estimation of relative uptake due to different tissue absorption of the 131I and 123I photons, nor by the radiation dose delivered by the 123I (European Journal of Nuclear Medicine and Molecular Imaging, June 2002, Vol.29:6, pp. 783-788).
In order to determine if 123I could potentially have the same stunning effects as 131I, very large doses would be necessary -- 100-300 mCi of 123I, equivalent to 1-3 mCi of 131I . Such an experiment has yet to be undertaken, Park said.
But Gerard said that the radiation burden to the thyroid is 100 times higher with 131I than with 123I. Gerard, Park, and other nuclear medicine specialists made their remarks during a presentation at the 2002 Society of Nuclear Medicine meeting in Los Angeles. The topic also was discussed at the October 2002 American Thyroid Association meeting, also in Los Angeles.
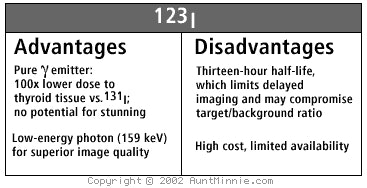
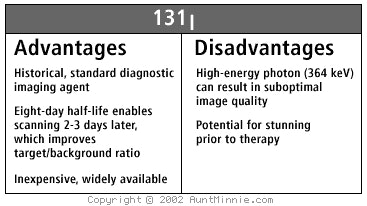
In his SNM presentation, Gerard reviewed the pros and cons of each of the iodine imaging agents.
 |
 |
Timing
Gerard touted the advantages of 123I, including optimal timing image acquisition, comparing 4-6, 24, and 48-hour imaging times. Although there are general guidelines about each of the three image-acquisition times, there is no final answer in terms of optimal timing, Gerard said.
 |
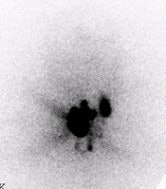
| Diagnostic anterior whole-body images taken with 131I, left, and 123I, right, of a 50-year-old male who was evaluated for sites of recurrent, differentiated thyroid cancer after 131I ablation. The body outline is easily identified in the 123I scan. Image courtesy of Dr. Stephen Gerard. |
Four to six hours offers the highest-count images and good sensitivity for detection of thyroid remnant, or the residual normal thyroid tissue following surgical thyroidectomy. A scan done at 24 hours after 123I administration resulted in better sensitivity for lower avidity thyroid tumor metastases.
Forty-eight-hour imaging has shown an improved target-to-background ratio and improved sensitivity in some cases, but it is more technically challenging, Gerard said. And while the 48-hour protocol may show additional lesions, including some less-avid thyroid metastases distant from thyroid bed, it may be unnecessary for simply defining the extent of thyroid remnant.
"The most definite thing that can be said about the timing for image quality is that 24 hours is superior to 6 hours," Gerard said.
At the SNM meeting Dr. Susan Mandel from the University of Pennsylvania in Philadelphia presented information about 5- and 24-hour use of 123I in imaging of patients with differentiated thyroid cancer (DTC).
The overall findings of this project indicated that scanning at 24 hours, after a 2.0-mCi dose of 123I as a diagnostic agent, is concordant with the post-131I therapy images in more than 90% of patients. This is very encouraging when the results are compared with those reported with diagnostic doses of 131I.
Mandel explained that 131I has traditionally been used for diagnostic imaging before 131I therapy, as well as post-therapy for surveillance of residual DTC. Although visualization of DTC is feasible with 131I, stunning may occur with diagnostic doses between 3-10 mCi.
Overall, Gerard and colleagues found that using 123I resulted in better image resolution compared with images obtained with the use of 131I.
Cost, availability, interest
Regardless of its clinical strengths, one major drawback of 123I might be the cost. At this point, it is estimated to be 3-4 times higher than 131I. Costs vary among vendors and institutions, but in one university lab, 3 mCi of 123I is approximately $150 more than 3 mCi of 131I, according to Park. However, the cost of 123I isn’t any higher than other new imaging agents, Gerard said. FDG typically costs $600 or more per dose, and most payors will reimburse for its use.
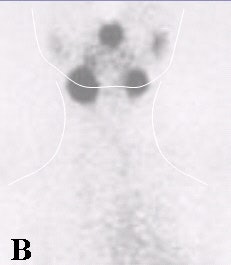
   |
| Diagnostic scans at 24 hours with 0.3 mCi 123I. No stunning effect is seen on these scans. Images courtesy of Dr. Hee Myung Park. |
Also at the SNM session, Dr. Edward Silberstein from the University of Cincinnati reported that the use of 123I is reimbursable using the thyroid carcinoma CPT codes, 78015 and 70818. Gerard noted that superior image quality helps justify the additional cost of 123I. Companies that market 123I, or Na-123I, include MDS-Nordion of Kanata, Ontario, Canada; Amersham Health of Princeton, NJ; Syncor International of Woodland Hills, CA; and Mallinckrodt of Hazelwood, MO.
But getting the nuclear medicine community on board the 123I train may not be so easy. Thus far, there has been resistance to 123I as an alternative. Nuclear medicine specialists would be wise to come around, according to Dr. Abass Alavi from the University of Pennsylvania.
Alavi and colleagues have examined over 400 patients after incorporating 123I into their clinical practice a few years ago, and the resulting images are impressive, he said. Working with this radioisotope takes some getting used to: For example, radioactive saliva in the esophagus can be a side effect of 123I, leading to false-positive results, Alavi said.
   |
| Post-therapeutic scans at 24 hours, and 7 days (last image) with 100 mCi 131I. These scans show excellent uptake of therapeutic dose. Images courtesy of Dr. Hee Myung Park. |
Alavi added that the half-life of 123I (13 hours compared to 8 days for 131I) and the fact that it only emits gamma rays by 123I (131I emits both gamma rays and beta particles) makes it less of a radiation risk.
Recently, Alavi and other University of Pennsylvania researchers have been experimenting with 123I doses up to 3-4 mCi, which is 10-15 times more than a conventional dose of 123I thyroid imaging.
In defense of 131I
Whatever its flaws, 131I is still the standard, and many nuclear medicine specialists feel that it will remain that way.
In a study from the Long Island Jewish Medical Center in New Hyde Park, NY, Dr. Salil Sarkar and colleagues questioned using 123I routinely in a clinical setting due to its lack of sensitivty for detecting thyroid cancer metastases.
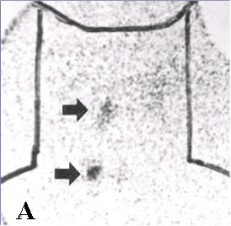
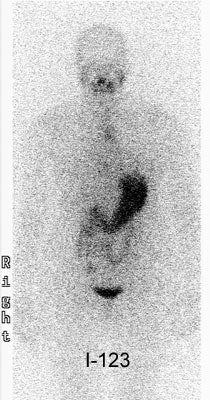 |
This patient had undergone thyroidectomy for papillary thyroid cancer and was presenting for evaluation prior to radioiodine ablation therapy. The patient had a thyroid-stimulating hormone (TSH) level of greater than 90. The diagnostic scan (above) was performed using 123I. The exam revealed no evidence of neck-bed activity and no metastases (the uptake in the chest was related to esophageal activity and cleared with water). Following treatment with 125 mCi of 131I, a 10-day post-therapy scan demonstrated a large amount of tracer activity in the thyroid bed and neck. Images courtesy of Dr. Scott Williams.
 |
For this study, 12 patients underwent 13 sets of pretherapeutic 123I and 131I studies. There were no metastases found in 6 patients on both imaging exams. Metastases were found in the remaining 6 patients; in 2 cases 131I showed diffuse pulmonary and cervical nodal metastases that were not seen on 123I images. In another patient, 131I indicated multiple skeletal lesions and diffuse pulmonary metastases, which were either not seen on 123I or seen only in retrospect (Journal of Nuclear Medicine, May 2002, Vol. 43:5, pp. 632-633).
No doubt some nuclear medicine specialists out there are taking a cue from Dr. Barry Siegel, chief of the division of nuclear medicine at the Mallinckrodt Institute of Radiology in St. Louis. Siegel’s approach to 123I is wait and see: The published data to date are good and suggest that 123I is at least comparable to 131I, he said.
However, Siegel is not quite ready to throw away 131I just yet: Cost is still an issue with 123I; the logistics of an 123I exam are more complicated; and it doesn’t allow for delayed imaging at 36 hours. "The whole issue of stunning is unresolved in my mind," Siegel added.
For others, there’s no question that the 123I has it. "It is about time that the medical community switch from 131I to 123I for all diagnostic purposes," Alavi said. "There is no question in my mind that 123I is the way to go."
By Laura RuthAuntMinnie.com contributing writer
October 21, 2002
Related Reading
Therapy-eluding metastases caught with FDG-PET, October 3, 2001
Risk of thyroid cancer doesn’t hinge on nodularity, April 17, 2001
Thyroid irradiation may be a risk factor for breast cancer, September 28, 2000
Copyright © 2002 AuntMinnie.com