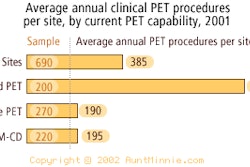
A new type of gamma camera designed specifically for breast imaging may improve the sensitivity of nuclear medicine in detecting breast cancer, an early study has found.
Led by Dr. Rachel Brem, researchers from the George Washington University Medical Center in Washington, DC, and the Johns Hopkins Institutions in Baltimore examined 50 patients with both a conventional gamma camera and the novel high-resolution breast-specific camera. The results are reported in the July issue of the Journal of Nuclear Medicine.
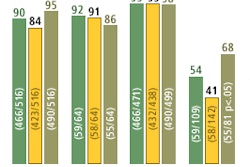
The sensitivity of scintimammographic cancer detection increased from 64.3% with the conventional camera to 78.6% with the breast-specific camera, the study found. The improvement was even greater with lesions smaller than 1 cm, where the sensitivity for breast cancer detection increased from 46.7% with the conventional camera to 66.6% with the breast-specific camera. The specificity remained constant between the cameras, at 93.3%.
All of the findings were confirmed by surgical or percutaneous biopsy. However, due to the limited number of patients involved, these differences did not achieve statistical significance, the authors wrote. A larger study that may confirm statistically significant differences is now under way.
The system used in the study is one of several breast-specific cameras in development around the world. This particular camera uses technology developed by the Thomas Jefferson National Accelerator Facility in Newport News, VA. The technology is now under license to Dilon Technologies of Newport News, a company in which Brem is a consultant and stockholder.
Use of gamma cameras for breast imaging is a relatively recent innovation that has provided physiologic information clarifying the benignity or malignancy of lesions in some patients, especially in women with dense breasts. However, the authors wrote, "(t)he design of a general-purpose gamma camera does not allow for optimal breast imaging and prohibits the acquisition of standard mammographic views that would allow better spatial registration between the modalities," (JNM, Vol. 43:7, pp. 909-915).
The study prototype differs from a conventional gamma camera in several ways. Instead of a single crystal, the prototype employs an array of 3 x 3 x 10 mm NaI (Tl) crystals separated by a 0.3-mm-wide reflective septum. According to the report, this pixel-based scintillator eliminates edge effects and allows the entire field of view to be useful.
 |
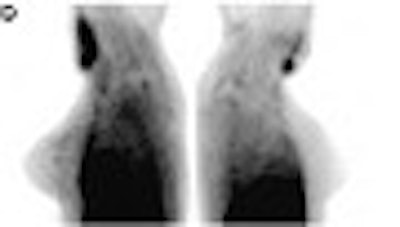
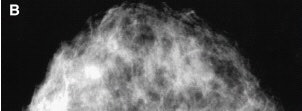
Detection of unsuspected cancer with high-resolution breast-specific gamma camera in 33-year-old woman, 2 years after lumpectomy and radiation therapy for infiltrating ductal carcinoma of the right breast. Mediolateral oblique and craniocaudal mammograms (A and B) of the left breast show normal findings.
 |
The high-resolution breast-specific gamma camera also allows imaging of seated patients, which has several advantages over the standard prone position, according to the authors.
"First, the patient’s arm can be positioned comfortably and need not be extended over the head," the authors said. "Second, the detector can be placed directly against the chest wall, providing better visualization of nearby tissue and allowing a full range of views -- craniocaudal, mediolateral, lateromedial, and oblique -- without interference from a table.
"Finally, the gamma-shield can be placed opposite the detector, and the distance between the detector and the breast lesion can be minimized by mild compression. This mild compression improves lesion contrast and background uniformity by minimizing breast thickness and providing a constant column height of tissue over the collimator."
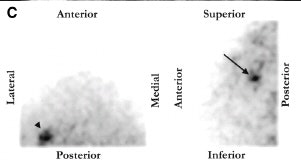 |
| Scintimammogram of the left breast (C) showed focal area of radiotracer uptake in upper (arrow) outer (arrowhead) quadrant. |
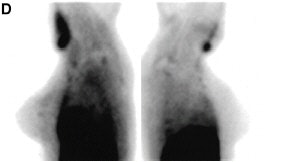 |
| Images taken with a conventional gamma camera (D) showed possible minimal radiotracer uptake in superior left breast. Biopsy revealed a 4-mm infiltrating ductal carcinoma. Images and captions republished with permission of the Society of Nuclear Medicine from Brem et al, July 2002, Vol. 43:7, pp. 909-915. |
Use of the prototype was not problem-free, however. Images of five patients obtained during the initial part of the study, when the camera was being modified, were excluded because of poor quality.
The initial study findings were welcomed in an accompanying commentary by Italian researchers. However, the commentators also stated that lesion detection with the new camera might have been better if imaging had been performed about 10 minutes after radiotracer injection, rather than being delayed until after the conventional camera scan, to nearly 90 minutes post-injection.
By Tracie L. ThompsonAuntMinnie.com contributing writer
August 6, 2002
Related Reading
Radiodetection may find more than one sentinel node, June 17, 2002
Scintimammography catches chemoresistance in breast cancer patients, June 13, 2002
Copyright © 2002 AuntMinnie.com