A number of recent studies have examined feasibility and patient acceptance issues associated with virtual colonoscopy screening for colorectal cancer. Researchers in Australia found good participation and acceptance in moderate-risk adults in a suburban screening population. Meanwhile, a group in Amsterdam examined the experiences of patients before, during, and five weeks after virtual colonoscopy. In both studies, individuals preferred VC over conventional colonoscopy.
As virtual colonoscopy practitioners fine-tune the technique in anticipation of building population-based screening programs, they are getting a good look at what works, what doesn't, and how patients feel about VC compared to the alternatives.
At the 2002 Virtual Colonoscopy Symposium in Boston, Dr. Richard Mendelson and colleagues from the Royal Perth Hospital and University of Western Australia in Perth presented the results of an ambitious community-based program to screen average-risk individuals for colorectal cancer.
"Funded by the Health Department of Western Australia, the aim of the study was to evaluate virtual colonoscopy as a tool for colorectal neoplasia screening in asymptomatic subjects, in relation to lesion detection, acceptability, and test accuracy, " Mendelson said.
Two thousand subjects were selected from an even mix of socioeconomic suburban backgrounds comprising two age groups: 52-54 and 65-69 years. There were three methods of recruitment. All subjects received a letter of introduction and invitation, followed up by phone call 3-4 weeks later. Subjects were excluded for known cancer, recent history of colonoscopy or barium enema, and other factors, leaving 1,471 eligible subjects, 28.4% of whom decided to participate.
"The commonest reasons given for nonparticipation were no time (23%), and the perception of good health and no need (17%)," Mendelson said, noting that there was no media or government-sponsored recruitment effort, and that participation compared favorably with that of other studies. The study found significantly higher participation among younger individuals, and among adults from wealthier suburbs.
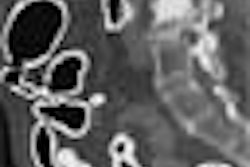
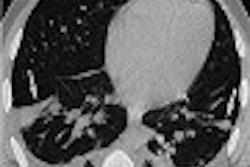
Virtual colonoscopy was performed in 340 individuals following standard bowel preparation and automated electronic bowel insufflation with CO2. All patients received buscopan antispasmodic unless it was contraindicated. CT images were acquired in both prone and supine positions using a standard low-dose CT protocol, including 70-mAs exposure.
An arbitrary decision was made to report any polyp 2 mm or greater, Mendelson said. Two experienced radiologists interpreted the results by consensus, examining 2-D axial images, then using multiplanar formatting and 3-D endoluminal reconstructions for problem solving. Results with one or more 2-mm polyps were deemed positive, and positive cases were referred for same-day colonoscopy.
Following the procedure, all of the patients were sent a questionnaire in the mail asking their opinions on the procedure.
"We looked at four parameters: pain, how subjects tolerated the procedure, general sort of nonspecific category of satisfaction, and the degree of embarrassment," Mendelson said. On a 100-point visual-analog (VAS) scale, participant satisfaction ran high. A score of 0 being best and 100 being worst, the median scores for pain, general satisfaction, embarrassment, and willingness to repeat screening were 14, 6, 8, and 5, respectively. Most subjects found virtual colonoscopy to be the same (32%) or better (61%) than expected, Mendelson said, while 6% found it worse than expected.
Virtual colonoscopy results were as follows. Polyps were detected in 93/340 (27.4%) of the individuals who underwent the procedures (123 total polyps), and the polyps were confirmed by conventional colonoscopy in 67/92 individuals who underwent both procedures. Virtual colonoscopy had an overall positive predictive value of 0.73.
The procedure's overall false-positive rate was 7.4% on a per-patient basis, with a positive predictive value of 0.74 for any polyp, and 0.55 for adenoma carcinoma. True sensitivity was impossible to determine, since individuals who had a negative VC did not proceed to optical colonoscopy.
"But in the 92 patients who had both procedures, virtual colonoscopy detected all of the lesions greater than 9 mm, including one case of asymptomatic rectal cancer, with lower sensitivity for lesions 6-9 mm, decreasing to 37% for lesions smaller than 6 mm," Mendelson said.
The referral of 27% of virtual colonoscopy patients to colonoscopy was troubling, however, as was VC's 7.4% false-positive rate, Mendelson said. But what it really boiled down to is the lack of standards for what constitutes a positive experience with virtual colonoscopy screening.
"So we looked at the effect of using a polyp-size threshold to determine what we were going to call a positive virtual colonoscopy, and (its) effect on the (7.4%) false-positive rate," he said.
However, adopting different criteria for what constitutes a "positive screening test" would have produced very different results. If a positive test had been defined as detection of a single polyp 5 mm or larger, or 2 polyps of any size, only 14% of VCs would have led to colonoscopy, and the false-positive rate for VC detecting a polyp would have been reduced to 4.2%. If only adenomas had been considered, the false-positive rate would have been 5.7%, and the colonoscopy referral rate would have declined from 27% to 14%, with no significant impairment of medium and large polyp detection.
"We need guidelines to be developed on what constitutes a positive colonoscopy," Mendelson said. "It is possible to develop these guidelines without compromising sensitivity or (missing) significant lesions."
He concluded that a community-based virtual colonoscopy screening study is feasible, has a high participation rate considering the lack of a media or physician-driven campaign, and that virtual colonoscopy results conform closely to those of conventional colonoscopy. The reasons for nonparticipation can be identified and targeted in future screening programs, he added.
"These data support virtual colonoscopy as an alternative colorectal cancer screening tool," Mendelson said.
In a later presentation, Dr. Jasper Florie and colleagues from Amsterdam's Academic Medical Center looked at long-term patient opinions on virtual colonoscopy versus conventional colonoscopy (CS) in 141 patients. Following standard bowel preparation, all of the patients underwent virtual colonoscopy imaging. Following administration of sedation or analgesics on request, the patients underwent CS.
Patients were asked to detail their experiences at four stages: before both procedures, after VC but before CS, after VC and CS, and five weeks after both procedures had been completed. Their responses are as follows:
Before any procedures. Bowel cleansing was feared most and virtual colonoscopy least. After bowel cleansing, 60% of the patients rated it moderately to severely burdensome.
After VC but before CS. 1.5% of the patients reported moderate-to-severe pain, 6% judged VC's overall burden to be moderate, and none rated it severe. Based on the patient literature provided, 86% of VC patients said the exam was no more burdensome than they had expected.
After CS. In all, 67% of CS patients received sedation, and 32% reported moderate-to-severe pain. The burden of CS was deemed to be moderate to severe in 57%. For their next screening exam, 75% of patients said they would prefer VC, 13% CS, and 12% had no preference, Florie said.
Five weeks later. Of the 90% of patients who returned the questionnaire, none reported having experienced severe pain with VC, 3% reported moderate-to-severe pain with the procedure, and 10% reported moderate pain. For most patients, insertion of the insufflation tube was the most burdensome aspect of VC.
With conventional colonoscopy, 32% of patients recalled having experienced moderate-to-severe pain, and 50% considered the procedure's overall burden as moderate to severe, Florie said, noting that insertion of the endoscope was the most burdensome aspect of CS.
Finally, 68% of patients preferred VC, 30% preferred CS, and 8% had no preference. Overall, colon cleansing was the most difficult part of the study. Patients experience less pain during VC than during CS. Immediately after the two procedures, patients strongly preferred VC over CS, but the strength of their preferences diminishes over time, Florie concluded.
A study published in June came to similar conclusions. Dr. M. Thomeer and colleagues from the University Hospitals in Leuven, Belgium examined 124 patients with both VC and CS, assessing patients' views after bowel purgation cleansing, after VC, and after CS. (European Radiology, June 2002, Vol. 12:6, pp. 1410-1415).
Overall, patients rated CS slightly less comfortable than VC, but the preparation was clearly the most uncomfortable part of the procedure, the authors wrote. As for preferences following both exams, 71% of the patients preferred VC, 24% CS, and 5% had no preference.
Interestingly, 28% of the patients liked VC better than CS even though they felt it was equally or even more uncomfortable than CS. The reasons included VC's faster procedure time, lower physical challenge (14 patients), and the lack of sedation (12 patients) associated with virtual colonoscopy.
Efforts to improve VC for patients should focus on techniques such as fecal tagging that might reduce or eliminate the need for bowel cleansing, the group concluded.
By Eric BarnesAuntMinnie.com staff writer
October 30, 2002
Related Reading
With similar treatment, blacks and whites with colon cancer fare equally well, August 14, 2002
In virtual colonoscopy, nothing beats a good prep, July 16, 2002
Recommendations on colon cancer screening updated, July 16, 2002
Routine colon cancer screening should start at age 50 for most people, June 7, 2002
Future looks bright for virtual colonoscopy, June 3, 2002
Copyright © 2002 AuntMinnie.com