As the healthcare facility of the future takes shape today, PACS is delivering more medical images to more categories of healthcare professionals. Organizations tasked with building and renovation are struggling to prepare for a future whose contours can be seen only hazily at best.
For the use of 3D and advanced visualization tools, however, a couple of trends seem clear: Radiologists are performing more interventional procedures, while surgeons and other subspecialists are spending more time looking at images -- both interoperatively to guide procedures with increasingly sophisticated systems, and for traditional preplanning and follow-up uses of medical imaging.
Creating an efficient operating or interventional suite that allows many different specialists to collaborate in using advanced imaging technologies is a complex but critical undertaking. To be useful, technology must answer the relevant and sometimes different questions of radiologists and surgeons, while integrating other professionals -- from cardiologists to nurses and technologists -- into the workflow in a way that allows them to do their jobs. The evolution isn't confined to the surgical suite. Even for day-to-day imaging and surgical planning, the ubiquity of PACS is changing the way specialists interact.
In talks at the 2007 Computer Assisted Radiology and Surgery (CARS) meeting in Berlin, researchers discussed the need to create a workable environment for interdisciplinary collaboration that addresses the needs of both the old and new players.
First, Elizabeth Beckmann, a partner with high-tech medical imaging consulting firm Lanmark in Beaconsfield, U.K., discussed the surgeon's needs for interpretation of radiological images. Then architect Bill Rostenberg, research director at San Francisco-based Anshen + Allen, talked about the workplace configurations that strive to accommodate the elusive practice of the future.
Seeing things differently
There is need to facilitate surgeons' interpretation of radiological images, Beckmann said. With the increasing dissemination of PACS throughout hospital departments comes an increasing awareness of the imaging information that's available and what information is available, including raw images, image databases, and "the increasing range of computer-based analysis that's available," she said.
"Historically, we've had the situation where surgeons had a different role -- they only had access to the paper (radiology) report and maybe the odd image," Beckmann said. "Any understanding they had about critical x-rays and other radiological images has come by default rather than by any structured learning. And there's a need for a greater understanding of what surgeons need to know about radiological images."
In England, specific issues make the need for increased access even more acute, namely a "tremendous amount" of outsourced imaging and diagnoses, she said.
"While PACS has increased the availability of images to surgeons and other key disciplines, the outsourcing is decreasing access to radiology professionals and specialists who need to answer questions the surgeons might have," Beckmann said. "So while surgeons do not need the ability to diagnose images, they do need to be able to interpret images. They need to improve their skills to have a better understanding of what they can get from the images. They need to know what information is available, what the different modalities need, and what is the optimal modality to be used for different procedures." And they need to know what kind of preplanning will give them the information they need.
The ability to give surgeons the right information at the right time will be critical to optimizing patient outcomes, Beckmann said. As a group their needs are unique.
"The world the surgeon lives in is a very different world than that of radiologists," Beckman said. Surgeons "have a different mind-set -- they think differently. They have a different skill set, and they actually view patient and medical information in a totally different way. They live in a 3D world, while traditionally radiologists largely have worked in a 2D world."
Radiological images are just one part of the information package surgeons need, she said, and unfortunately, it has been difficult for surgeons to get the training they need, since learning materials are overwhelmingly geared toward radiologists.
"Surgeons need to know what the surgical implications are of the images they're looking at, what the surrounding anatomy is like," Beckmann said. From the images, they need to know what's behind the area they're operating on, the significance of the grayscale, when to order x-ray versus MRI versus CT.
In short, "we must tailor a knowledge pathway for each discipline," taking into account the different mind-set of surgeons, Beckmann said.
"The ongoing challenge is how to achieve this in a setting that demands both increased effectiveness and efficiency, and also allows far less time now for learning than it used to," she said. "If we get learning for surgeons right, we will optimize surgical planning. If we get it wrong, we may have some rather sad effects."
The evolving OR
Today, there is a melding of the once-separate kingdoms of surgery, imaging, and cardiology, Rostenberg said in his CARS presentation.
"It's no secret that interventional procedures and surgical procedures have not only changed radically in recent decades, but in many ways are converging and becoming more similar," he said. "My profession has typically designed surgical suites one way and interventional radiology suites another way.... Does that really make sense for both surgery and interventional radiology?"
In terms of facility requirements, an increasing reliance on image guidance means a greater need for PACS, and also a greater need to interact with images in the surgical suite, said Rostenberg, an architect who has authored several books on the design and planning of healthcare facilities. Rostenberg is also a guest instructor at both the Harvard University Graduate School of Design and the Radiological Society of North America (RSNA).
While there is a clear need for more information technology throughout the healthcare enterprise, both with regard to equipment and data, in the OR there is generally no place to put extra equipment -- or the increasing numbers of nonsurgical professionals needed to operate it and monitor procedures.
"We're seeing not only more people but different types of people in surgical suite, whether it's technologists to run the advanced radiology equipment used for guidance, or someone to be able manage the interpretation of advanced imaging and information data generated in the surgical suite," Rothenberg said. Interventional radiologists and cardiologists are coming into the OR, too, he said. As time goes on, there is less and less difference between the surgical and radiology suites.
Indeed, radical changes are taking place in the control and flow of materials as procedures become more interventional, Rostenberg said. Both operating rooms and interventional suites are using more images, though it's been difficult to see the images, particularly in the invasive surgery setting when the rooms are darkened.
As a potential solution, the integrated imaging suite can relieve staffing shortages, accommodate new types of personnel, maintain individual equipment service lines and brand identities, while reducing the politics, cultural, and turf battles that can impede cooperation and workflow in some facilities.
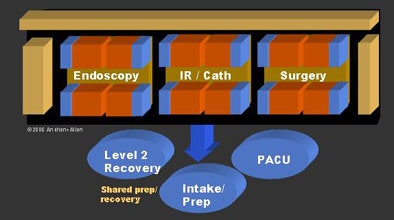 |
| The integrated interventional suite refers to the consolidation of various interventional services within a common area and operated as an integrated program. It is designed to accommodate future changes in medical practice and technology by modularizing both procedure rooms and pods of rooms. In doing so, it creates maximum flexibility with a minimum of changes to the physical facility. Image © Anshen + Allen Architects. |
To counter the effects of screen glare in darkened surgical suites, some facilities are using green ambient lighting in the OR, Rostenberg said. The green light solution, which may have been pioneered on submarines, he said, has generated much anecdotal discussion but to date little hard research proving its effectiveness.
 |
| Green light ambiance in a surgical suite at the University of California, Los Angeles is created by placing theatrical green gel over ambient fluorescent lighting. Green lighting may reduce glare and increase sharpness of flat-panel monitors compared to a darkened room. Photos by Bill Rostenberg, FAIA, FACHA, principal Anshen + Allen. |
Placing the hardware that provides the data in the OR has been difficult, Rostenberg said. Most ORs aren't designed like cath labs or angiography suites that are equipped with an electronics room or control room -- there hasn't been space.
"What we're doing is designing surgical suites that are either designed with control rooms or ... able to incorporate them in near future," Rostenberg said. "The most common request I'll get in a new hospital is for someone in surgery to say, 'We're not ready yet, but because we're investing all this money in a new facility, I want you to design a new suite to incorporate intraoperative MRI -- and I don't know what type we're going to use.' "
There are many configurations to choose from for intraoperative MRI, he said. The simplest, from an architectural viewpoint, is a stationary permanent magnet sited in an alcove, though the equipment can also be made portable, Rostenberg said.
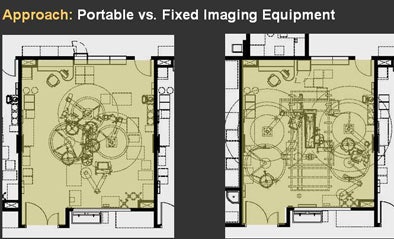 |
| "Universal" or interchangeable operating rooms were designed to accommodate both fixed and portable imaging equipment. Rooms with portable equipment (left) are more flexible, while those with fixed equipment (right) tend to be more dedicated to certain specialties. Image © Anshen + Allen, Associated Architects for Palomar Pomerado Health. |
Another idea improves the use of space by combining surgical prep and recovery in a single room set off from the interventional suite. One design utilizes a modular approach to solve the problem of different space needs for different procedures.
 |
| Palomar West Medical Center exemplifies the integrated interventional suite concept, while also introducing an abundance of daylight into complex surgical and interventional imaging departments that are traditionally dark. Image © Anshen + Allen, Associated Architects for Palomar Pomerado Health. |
The modular set-up can be used for interventional radiology and cardiology electrophysiology studies, as well as well as surgery, and includes a small area for endoscopy, Rostenberg explained.
A smaller area designed as flexible modules includes OR modules that are identical in shape and size to interventional radiology modules, but used very differently. To accommodate MRI, a room or pair of rooms are identified as the safety zone to prevent unauthorized entry. Determining which staff will be placed in the core room for which procedures has been one of the most difficult issues, he said.
 |
| While pods of procedure rooms are geometrically "regularized," they are also operationally differentiated. In this example, surgical operating rooms are placed around a central clean core, while interventional radiology and cardiology procedure rooms are placed around a central work core. Thus, the workflow of one pod is very different from that of the other. |
The process of integrating new designs really requires a long look into the future at a "new operational model," Rostenberg said. "It's a once-in-a-lifetime opportunity to design a new hospital and not duplicate (existing) operational and territorial issues," he said. "This concept only works when there is that kind of support from the executive suite."
By Eric Barnes
AuntMinnie.com staff writer
November 5, 2007
Related Reading
Advanced liver imaging shapes surgical strategies, September 18, 2007
MDCT's 'virtual Whipple' offers practice run before complex surgery, August 16, 2007
CARS news: Automated device tracking beats conventional CT/US guidance, June 28, 2007
Part III: Image processing has room to grow, October 23, 2006
CARS suite of the future sees key role for image-guided intervention, June 23, 2005
Copyright © 2007 AuntMinnie.com