With all the controversy stirring in venous ultrasound, it's not always easy to decide the best way to conduct, read, or follow up on exams. But in a talk at the 2003 Leading Edge in Diagnostic Ultrasound meeting in Philadelphia, Thomas Jefferson University’s Dr. Laurence Needleman put matters in perspective with his overview of the thorniest issues in venous ultrasound.
Calf vein imaging
Approximately 17% of symptomatic deep venous thrombosis (DVT) patients have isolated calf DVT, with varying frequency depending on who is sent for the study. Assuming an incidence of DVT of 25%, approximately 4% of patients have isolated calf DVT, said Needleman, an associate professor of radiology at the Philadelphia-based university.
The American College of Radiology (ACR) and the American Institute for Ultrasound in Medicine (AIUM) differ on the need for ultrasound of calf veins, however, Needleman said.
The ACR leaves it as an optional decision, while the AIUM states in a standard, "The calf veins should be imaged in at least the transverse view. Real-time imaging should be performed with and without pressure applied on the skin in an effort to completely appose the walls of the vein..."
There’s also no consensus on a protocol for calf vein imaging. According to an AIUM standard, "Imaging of the full extent of these veins should be attempted. Views of the lower extremity veins should include transverse images of the peroneal, posterior tibial, anterior tibial, and, when possible, muscular veins." The ACR standard does not discuss protocol.
The reality of calf vein imaging is that anterior tibial vein (ATV) thrombosis is rare, and ATV is frequently eliminated, Needleman said. Most protocols evaluate paired veins (posterior tibial and peroneal veins), while some scan from one position (medial calf). Other protocols scan from two positions (one for PTVs, one for peroneals), while others attempt to scan gastrocnemius and soleal veins separately, he said.
Most labs, though, attempt to visualize PTV and peroneal veins from one position (in near and far field, respectively).
As for the clinical significance of calf vein thrombosis, most feel that isolated CVT does not cause symptomatic pulmonary embolism. Instead, the clot continues to develop in the more proximal veins and embolize to cause PE, he said.
While isolated calf clot is found in PE patients, that could have been left behind after the bigger clot embolized in a bigger vein and is actually not CVT. In some research studies, patients with isolated calf clot were found more likely to develop more proximal DVT and reflux in months following the DVT, Needleman said.
"This has been an impetus for people to treat people with isolated calf DVT," he said.
The American College of Chest Physicians (ACCP) recommends treatment of symptomatic calf vein thrombosis if there isn’t a contraindication, Needleman said.
Needleman noted that calf vein imaging is increasing, and more physicians are interested in the studies. It’s good practice to scan symptomatic areas whether or not calf veins are studied, he said.
If patients present with calf pain and the proximal veins (popliteal vein and above) are free of disease, the symptomatic region should be scanned, Needleman said.
"If you don’t know what you’re looking at, if you don’t know if it’s a mass or a hematoma or a tumor or Baker’s cyst, fine, send it to somebody who does know how to interpret it," he said. "But it’s probably more important for you to say, there is an abnormality…and get the patient moved on with a presumptive diagnosis that something’s wrong there that may be an important part of the diagnosis."
Bilateral versus unilateral studies
There is consensus that spectral Doppler studies should be performed on both common femoral veins, as symmetry is important to diagnose unilateral iliac obstruction. If spectral Doppler is viewed as an important criterion for accurate diagnosis, using symmetry between sides becomes more important, Needleman said.
Is it necessary to perform a study on both limbs?
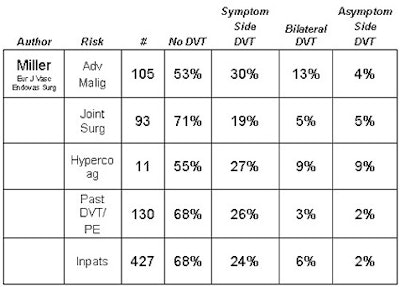
"I feel high-risk patients who are likely to have asymptomatic disease should have both legs scanned," he said. "This includes trauma patients and those with hypercoagulable states. Since many inpatients develop PE without preexisting symptoms, our lab performs bilateral studies on all inpatients." But the literature also supports performing only unilateral studies, he added.
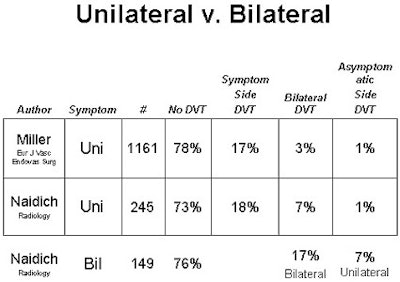 |
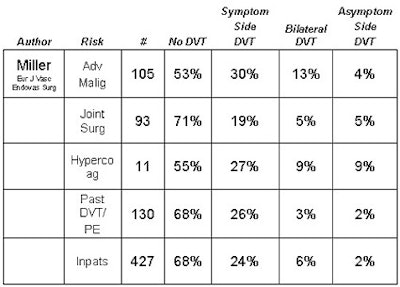 Charts courtesy of Dr. Laurence Needleman. |
The contralateral common femoral vein (CFV) should be studied in patients with a newly diagnosed clot in one leg, in case an IVC is placed, Needleman said.
"We generally perform a bilateral study in case the patient presents in the future with symptoms on the other side," he said. "This creates a baseline to determine if there was asymptomatic DVT or scarring on the asymptomatic side."
Patients with bilateral symptoms should receive bilateral studies, as many patients will have congestive heart failure (CHF), Needleman said.
At Needleman’s lab, most patients get bilateral studies. Outpatients who have no cancer, have been on bed rest less than four days, have no known hypercoagulable state, and no significant trauma get unilateral exams, he said.
While there is evidence that ultrasound screening of some high-risk groups may reduce the risk of PE, this may be affected by the widespread use of compression boots, Needleman said. As a result, the reasonableness of performing a study on asymptomatic patients is still open to debate.
Also, ultrasound for screening purposes is not accepted for billing by most carriers. Most screening tests are performed in hospitalized patients because physicians find value in the procedure, even if insurers don’t, Needleman said.
US for suspected PE?
Ultrasound is sometimes considered in this application, as PE is presumed if there’s a positive ultrasound along with chest symptoms. A normal ultrasound does not rule out PE, however.
As a result, Needleman believes that the best approach is to first perform a lung study, such as a nuclear scan, CT, or, with less frequency these days, pulmonary arteriography.
US may be considered in situations such as:
- Other studies for PE are not immediately available, but ultrasound is.
- Patients with a contrast allergy where the ventilation perfusion (VQ) scan is equivocal (intermediate, indeterminate, or even low-risk) or if there is high clinical suspicion.
- Patients with unilateral symptoms (patients with bilateral symptoms are less likely to have DVT).
Some groups turn to ultrasound for any patient having an equivocal scan, Needleman said.
"My own preference is to go straight to CT angiography," he said.
FUO
For patients with a fever of unknown origin (FUO), venous ultrasound may be indicated. A 1997 study found that 6% of patients had a DVT that explained their symptoms. This diagnosis was obtained at an average cost for each detected DVT case of $10,260 (Surgery, April 1997, Vol. 121:4, pp. 366-371).
"This (DVT rate) is higher than my own experience, and it likely represents the fact that most patients I see are referred for fever -- not FUO," he said. "If a patient truly has a FUO, a venous US may be warranted."
Therapy
It’s easy to get into trouble if the patient is examined during initial treatment with heparin, Needleman said. DVT may change, and even extend on adequate heparin therapy, and this is not a reason in itself to place an inferior vena caval (IVC) filter.
"The fact that you’ve showed that the clot is bigger on a follow-up study is not an indication in and of itself to put a filter in," he said. "Repeating an ultrasound just to see how the clot is doing is kind of like doing a chest x-ray to see if the pneumonia is dissolving. It’s really not necessarily good medicine, and what patients really need are blood tests that show they’re adequately anticoagulated, and that the blood tests be carefully monitored."
The ACCP recommendation for IVC filters is as follows:
"We recommend placement of an inferior vena caval filter when there is a contraindication or complication of anticoagulant therapy in an individual with or at high risk for proximal vein thrombosis or PE. We also recommend placement of an inferior vena caval filter for recurrent thromboembolism that occurs despite adequate anticoagulation, for chronic recurrent embolism with pulmonary hypertension, and with the concurrent performance of surgical pulmonary embolectomy or thromboendarterectomy" (Chest, Jan 2000, Vol. 119:1 supplement, pp. 176S-193S).
Patients on warfarin therapy may develop new DVT, and therefore may require an ultrasound if there are any new symptoms, which requires a change in therapy back to heparin, he said.
"In my experience, this may be true in cancer patients and others who have a particularly aggressive hypercoagulable state," he said.
Ultrasound is underutilized, however, at the end of therapy, Needleman said.
It’s helpful to identify the approximately 50% of patients who have scarring at the end of therapy. And if patients return with symptoms, findings can be compared to the appearance post-therapy, he said.
Recurrent DVT is one of the most challenging diagnoses in venous ultrasound, and having a comparison can make this task easier, he said. A new, noncompressible vein or a scarred vein that compresses less than before generally indicates new disease.
24/7 availability
The need to make venous ultrasound constantly available is a controversial topic. If sonographers are in-house 24/7, studies should be performed when they are ordered, Needleman said.
However, most institutions do not enjoy such a setup. Some emergency rooms treat some patients with low molecular-weight heparin, and have the patient come back or wait until the following morning for ultrasound. Patients with a contraindication to anticoagulation need the study soon after the test is ordered, however, Needleman said.
As described in an internal TJU document, contraindications to anticoagulation include:
- Heme-positive stool.
- Ulcers less than six weeks old.
- Hemoglobin below seven grams.
- CNS surgery within 10 days.
- Closed head injury less than 10 days old.
- Stroke less than three weeks old.
At TJU, sonographers perform routine ultrasound from 6:30 a.m. to 9:30 p.m., with house staff performing scans during off-hours, Needleman said.
One study or serial studies?
If the calf vein is not evaluated, follow-up may be needed in five to seven days, he said. If CVT is identified and not treated, Needleman recommends followup until resolution or for 10-14 days (per ACCP recommendation).
From published studies, Needleman has concluded that two studies five to seven days apart are definitely adequate to exclude DVT, and that the value of one "complete" examination is not entirely proven.
By Erik L. RidleyAuntMinnie.com staff writer
August 28, 2003
Related Reading
FDG-PET, scintigraphy offer a break in fever of unknown origin, August 22, 2003
US can confirm if surgery is right for popliteal artery aneurysm, August 5, 2003
Venous Catheters: A Practical Manual, July 22, 2003
No need to include calf in sonographic DVT assessment, May 5, 2003
US-guided laser offers effective treatment for varicose veins, April 25, 2003
New techniques increase ultrasound’s value in vascular imaging, July 8, 2002
Copyright © 2003 AuntMinnie.com




















